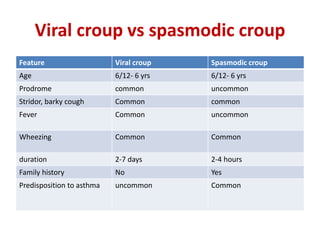
Croup is a common viral illness affecting children aged 6 months to 6 years, characterized by symptoms such as a barking cough, hoarse voice, and inspiratory stridor. The condition is primarily caused by parainfluenza viruses and typically resolves within a week, although complications can occur in about 15% of cases. Management focuses on airway maintenance with treatments including corticosteroids, mist therapy, and racemic epinephrine.