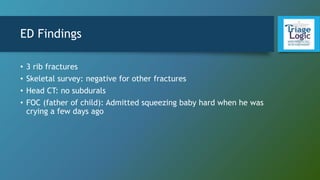
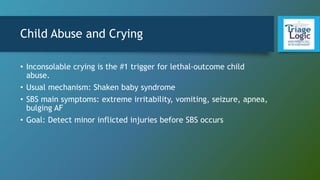
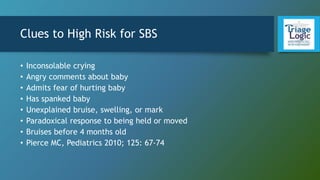
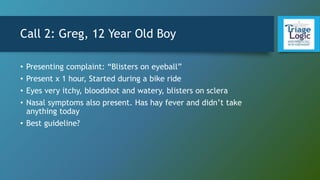
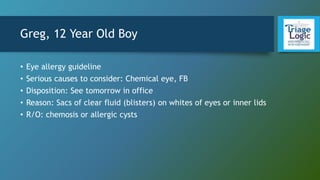
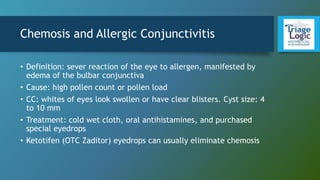
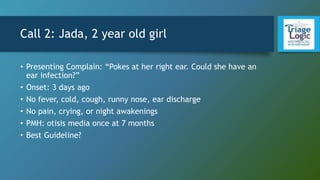
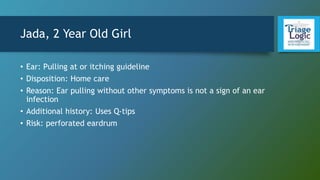
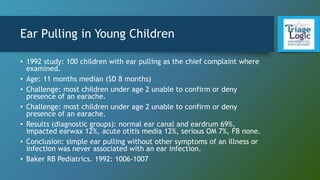
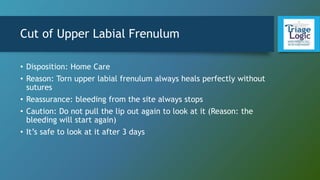
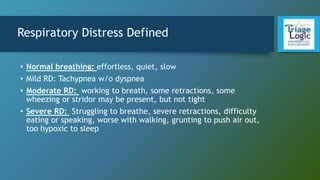
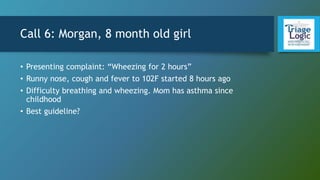
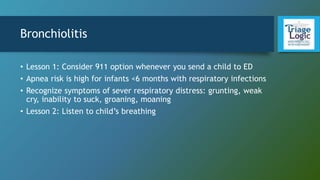
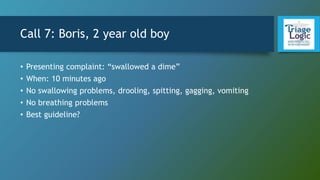
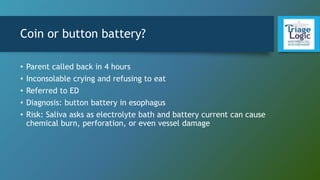
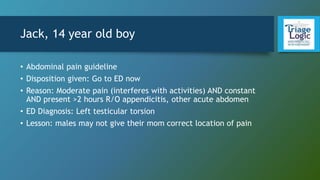
The document provides guidance on choosing protocols and dispositions for various pediatric patient cases presented to a telehealth triage nurse. It describes 9 calls involving children with various complaints such as crying, eye irritation, ear pulling, mouth bleeding, wheezing, swallowed objects, abdominal pain, limited arm movement, and provides the guidelines and rationales chosen by the nurse. It emphasizes the importance of actively ruling out serious conditions, considering 911 in some respiratory cases, and giving instructions to reduce injuries like subluxed joints if emergency department access is not possible.