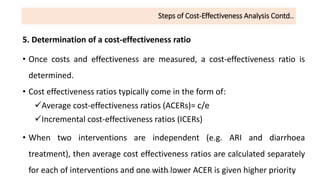
Cost-effectiveness analysis (CEA) evaluates the costs and health outcomes of health interventions to determine their efficiency in terms of cost per health outcome achieved. It helps decision-makers prioritize interventions based on their health benefits relative to costs, considering different perspectives and alternatives. While CEA is useful for technical efficiency and prioritization, it has limitations, such as not accounting for social desirability and equity aspects of health outcomes.