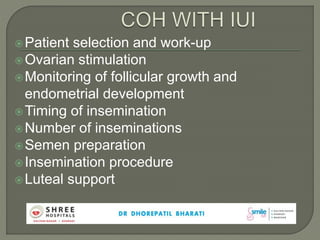
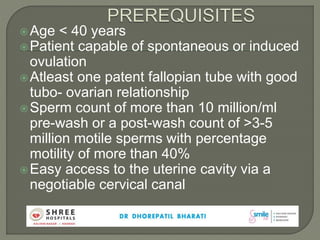
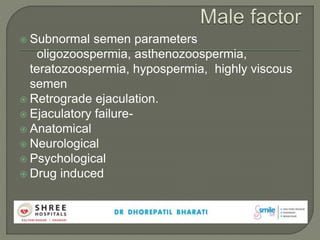
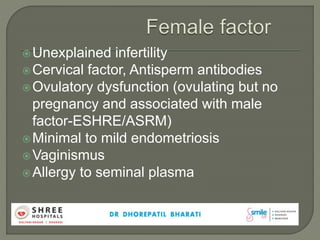
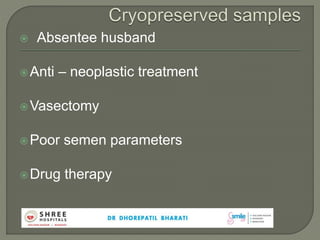
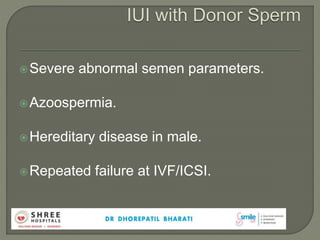
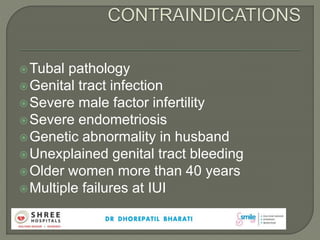
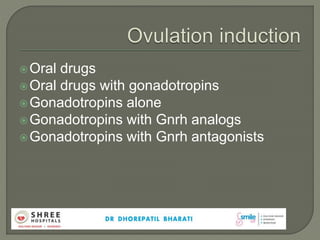
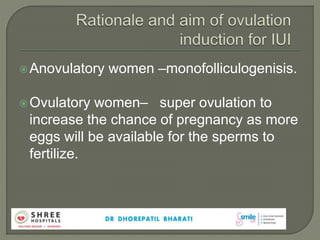
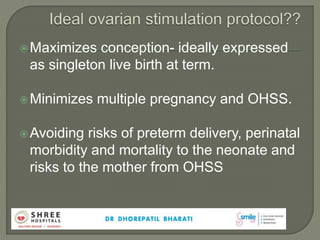
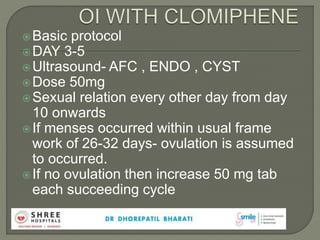
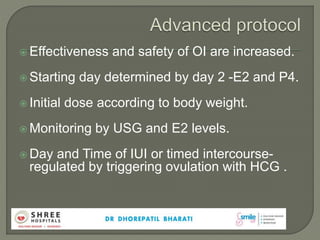
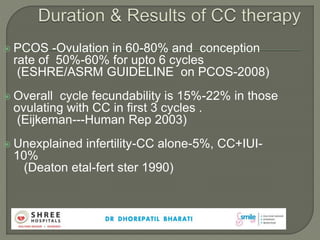
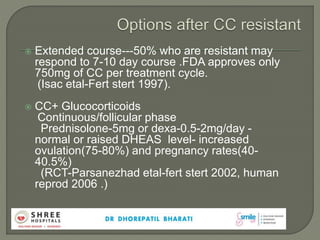
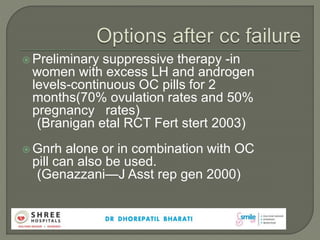
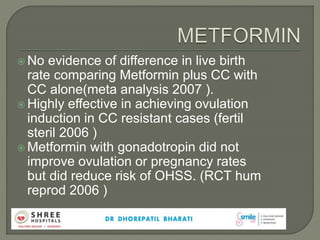
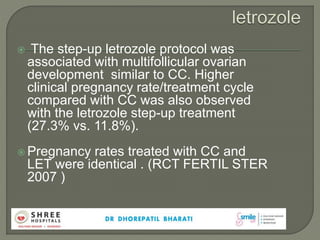
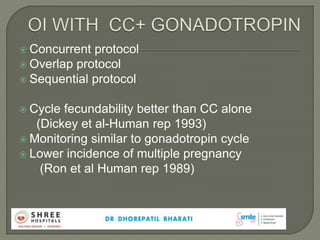
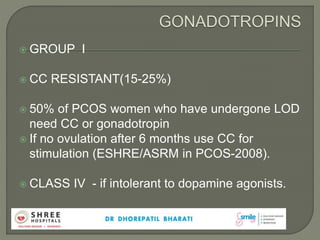
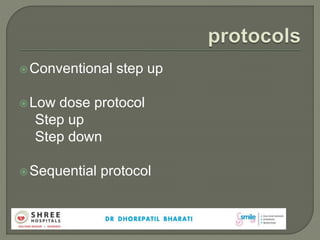
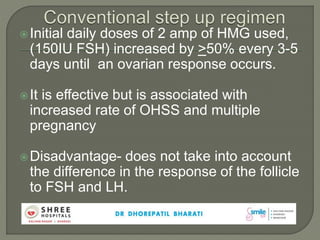
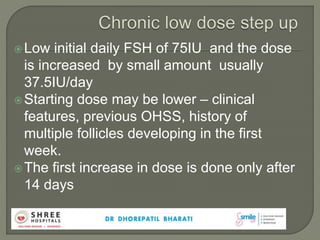
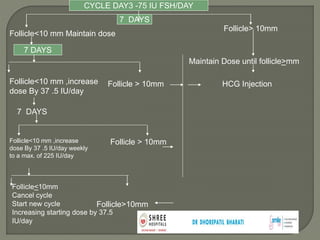
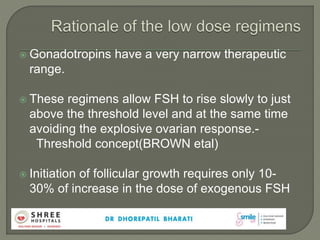
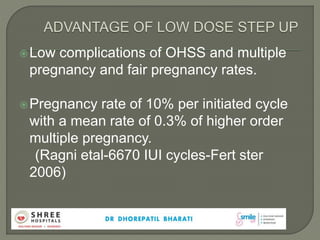
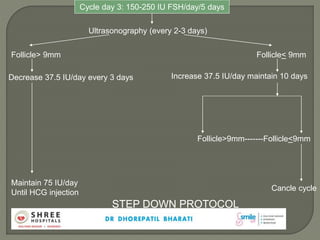
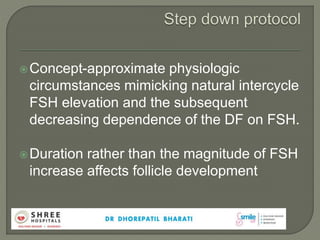
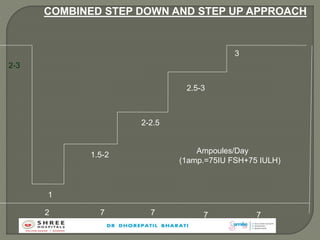
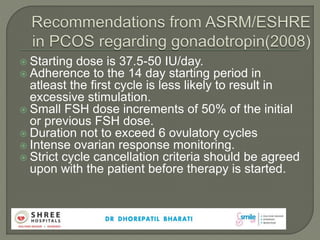
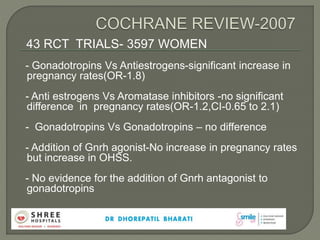
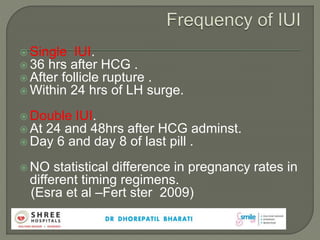
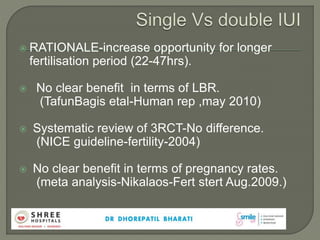
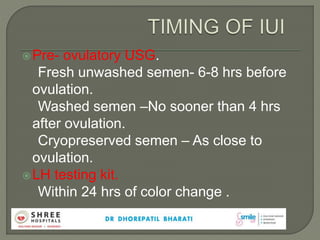
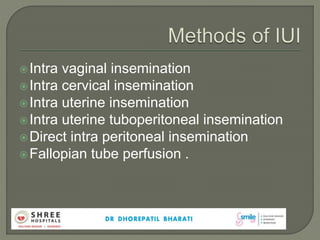
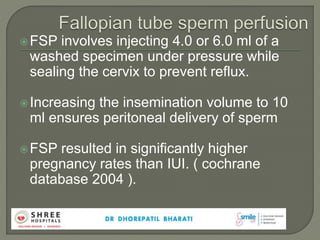
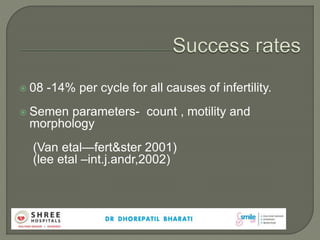
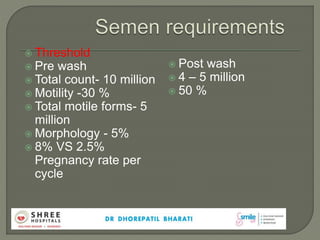
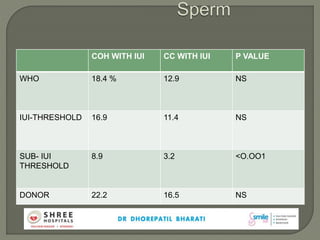
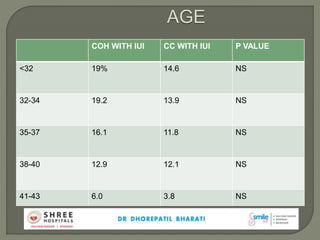
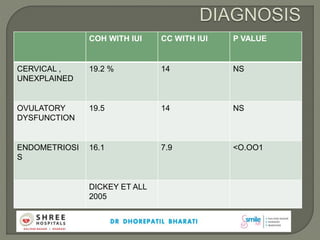
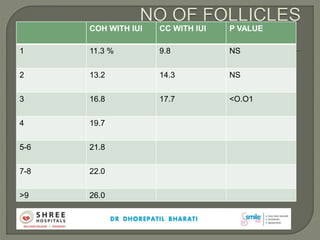
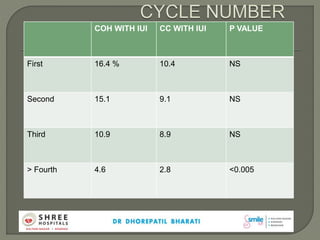
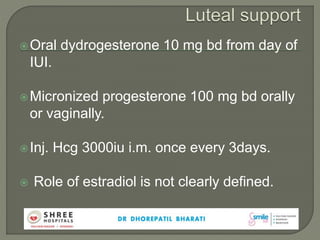
The document outlines protocols for ovarian stimulation, insemination procedures, and patient selection criteria in infertility treatments, particularly focusing on intrauterine insemination (IUI) and ovulation induction methods. It discusses various patient factors affecting treatment outcomes, such as age, semen quality, and underlying infertility causes, while emphasizing the effectiveness of different drug regimens. Additionally, it presents data on pregnancy rates and the relative advantages of different treatment protocols, highlighting the importance of personalized approaches in addressing infertility.