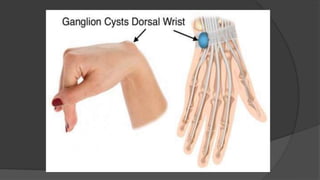
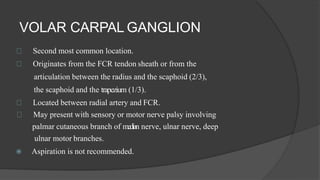
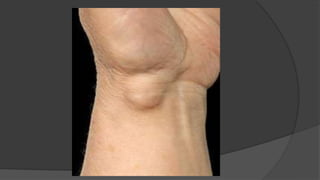
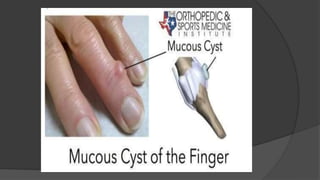
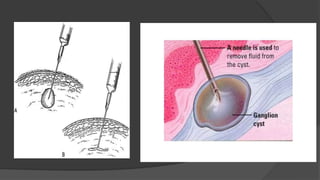
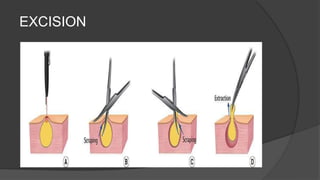
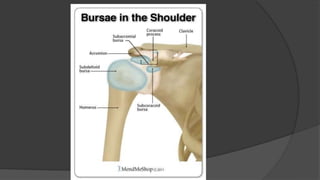
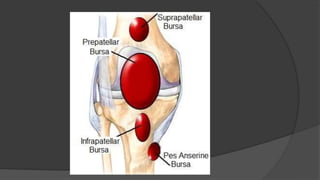
This document discusses ganglion cysts. It begins with an introduction stating that ganglion cysts are common wrist swellings caused by leakage of synovial fluid. It then discusses the locations where ganglions commonly appear and potential etiologies. The document continues exploring the pathology, pathogenesis, clinical features, different types of ganglion cysts, differential diagnosis, treatment options which include observation, aspiration and excision, rehabilitation process and potential complications. It concludes with briefly discussing bursae, bursitis and their treatment.