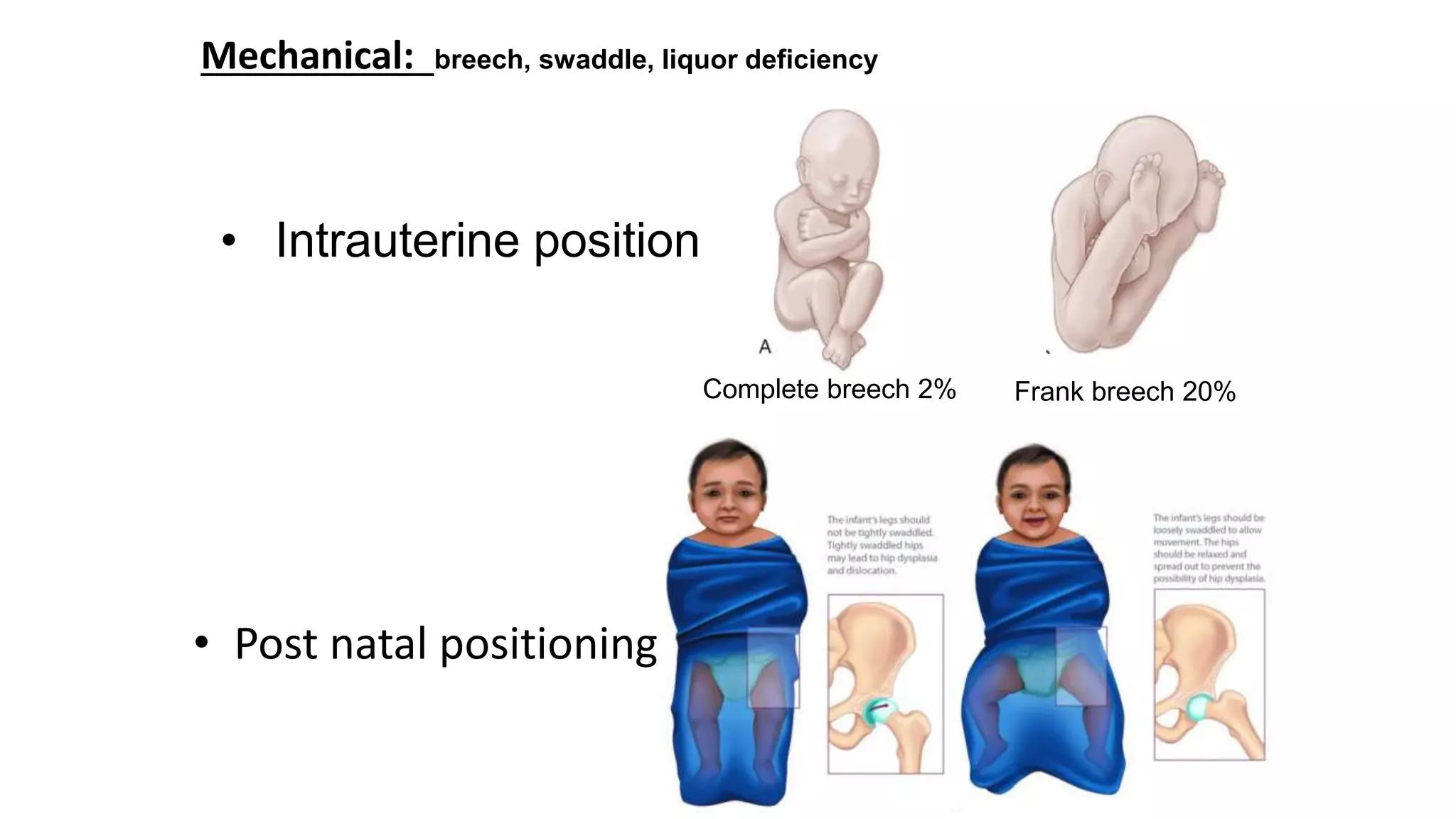
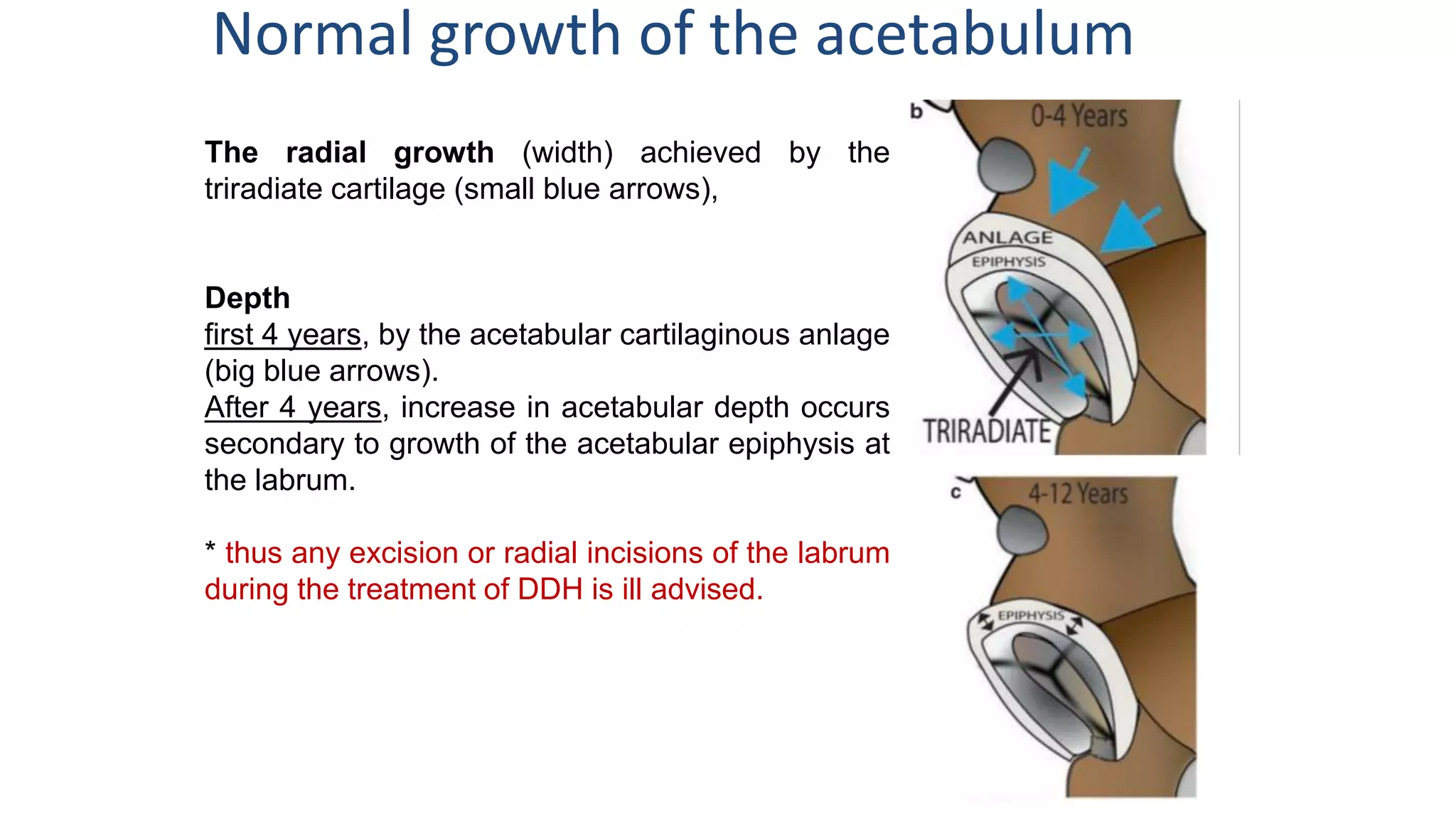
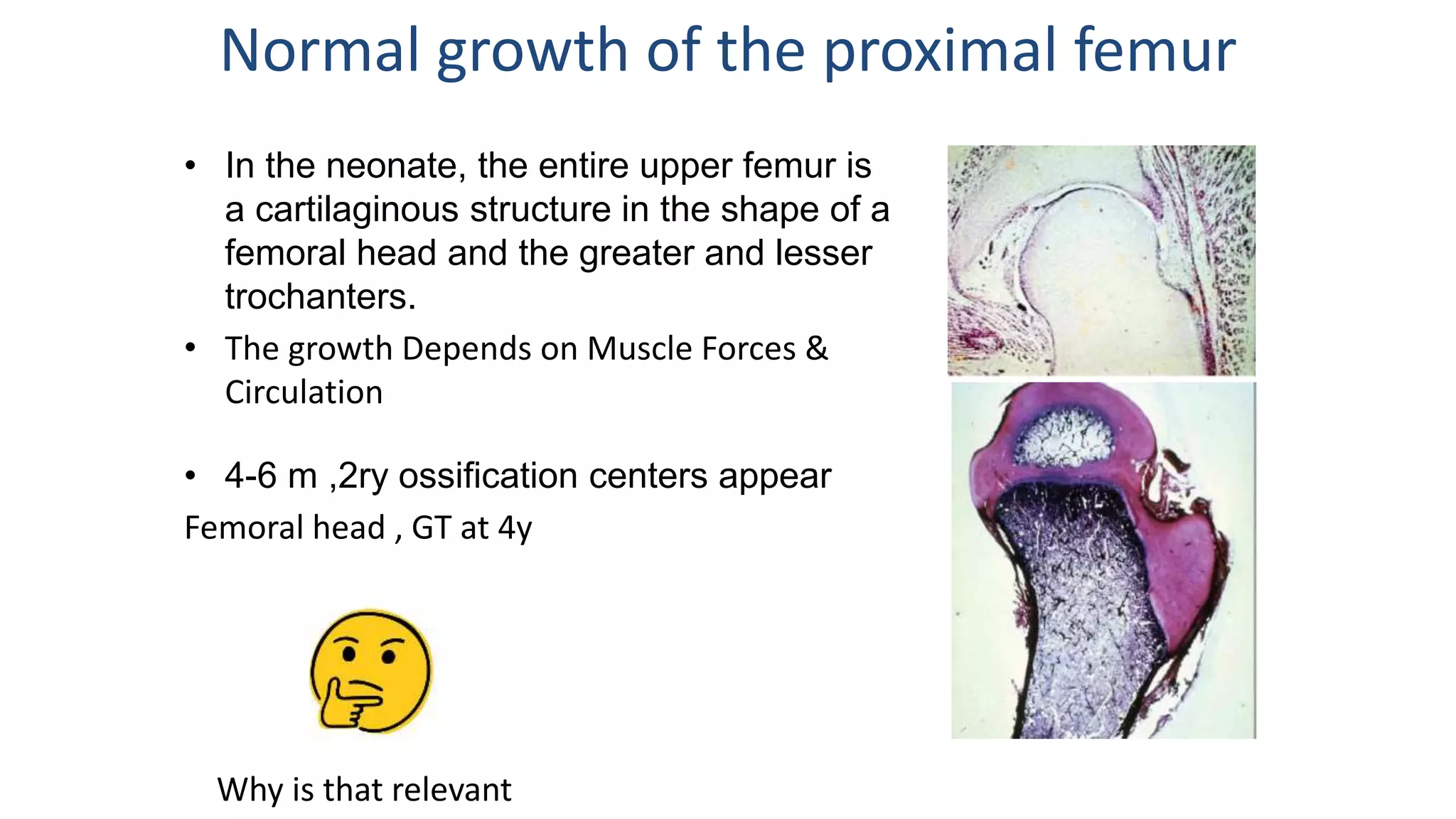
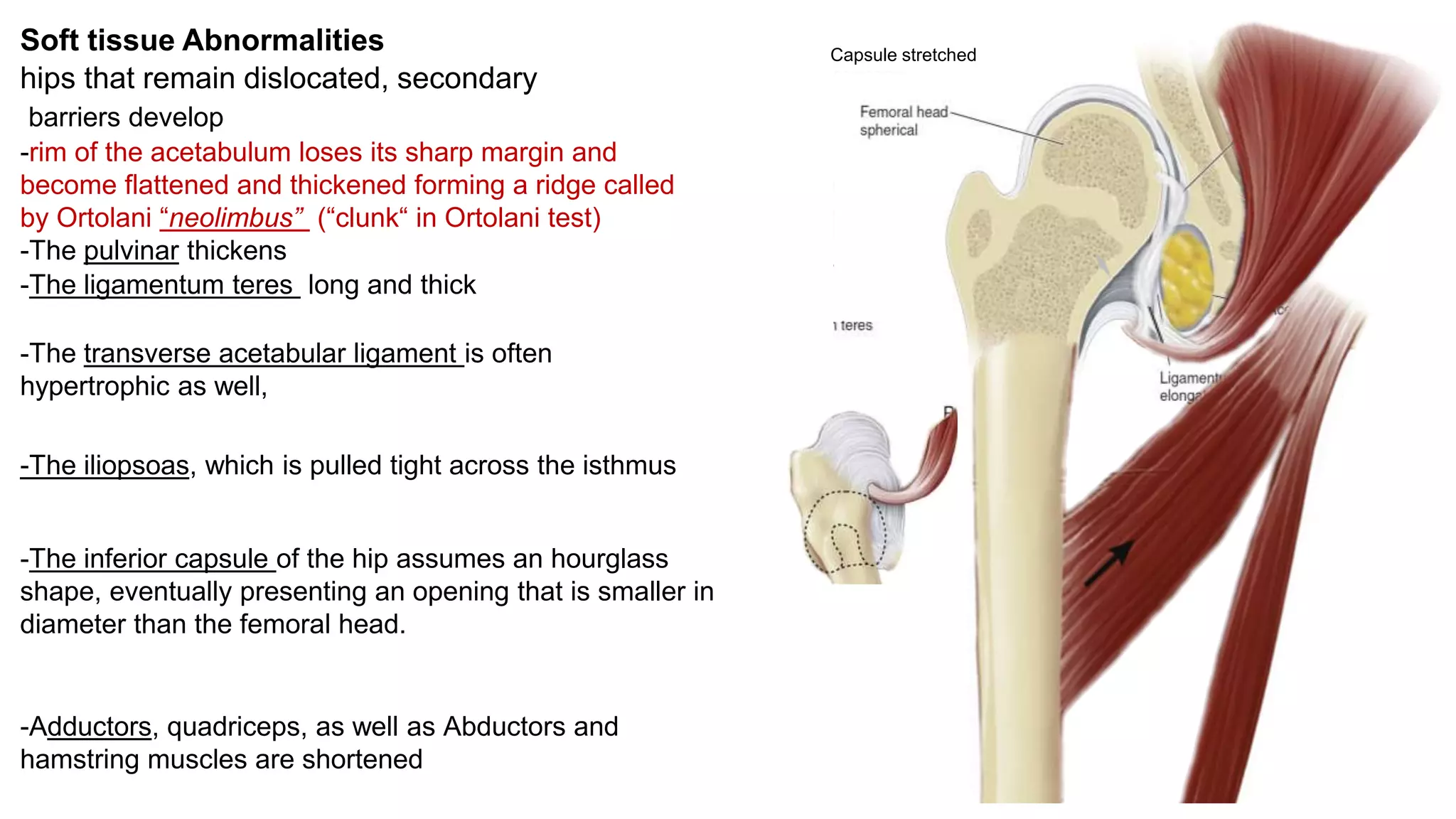
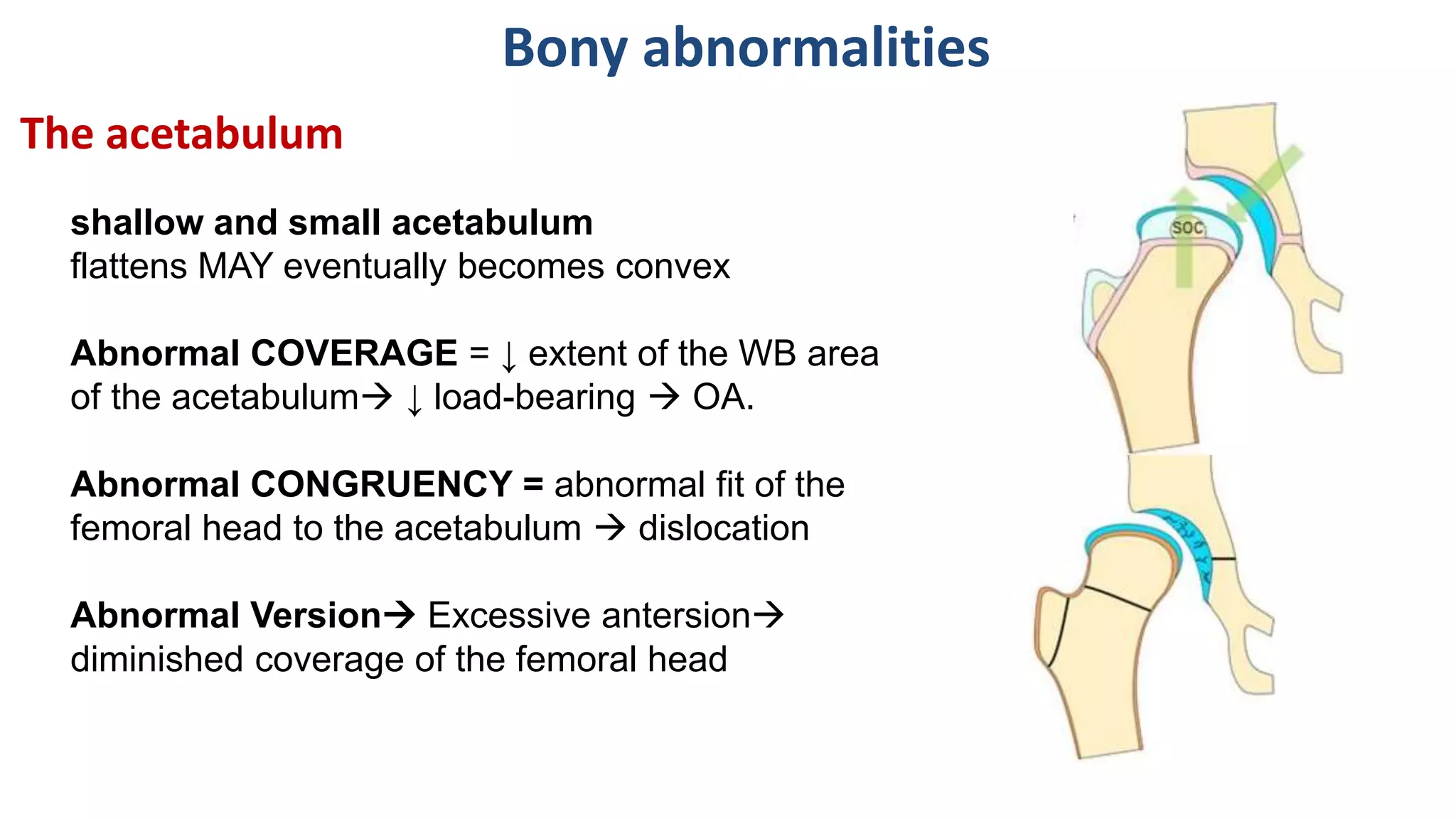
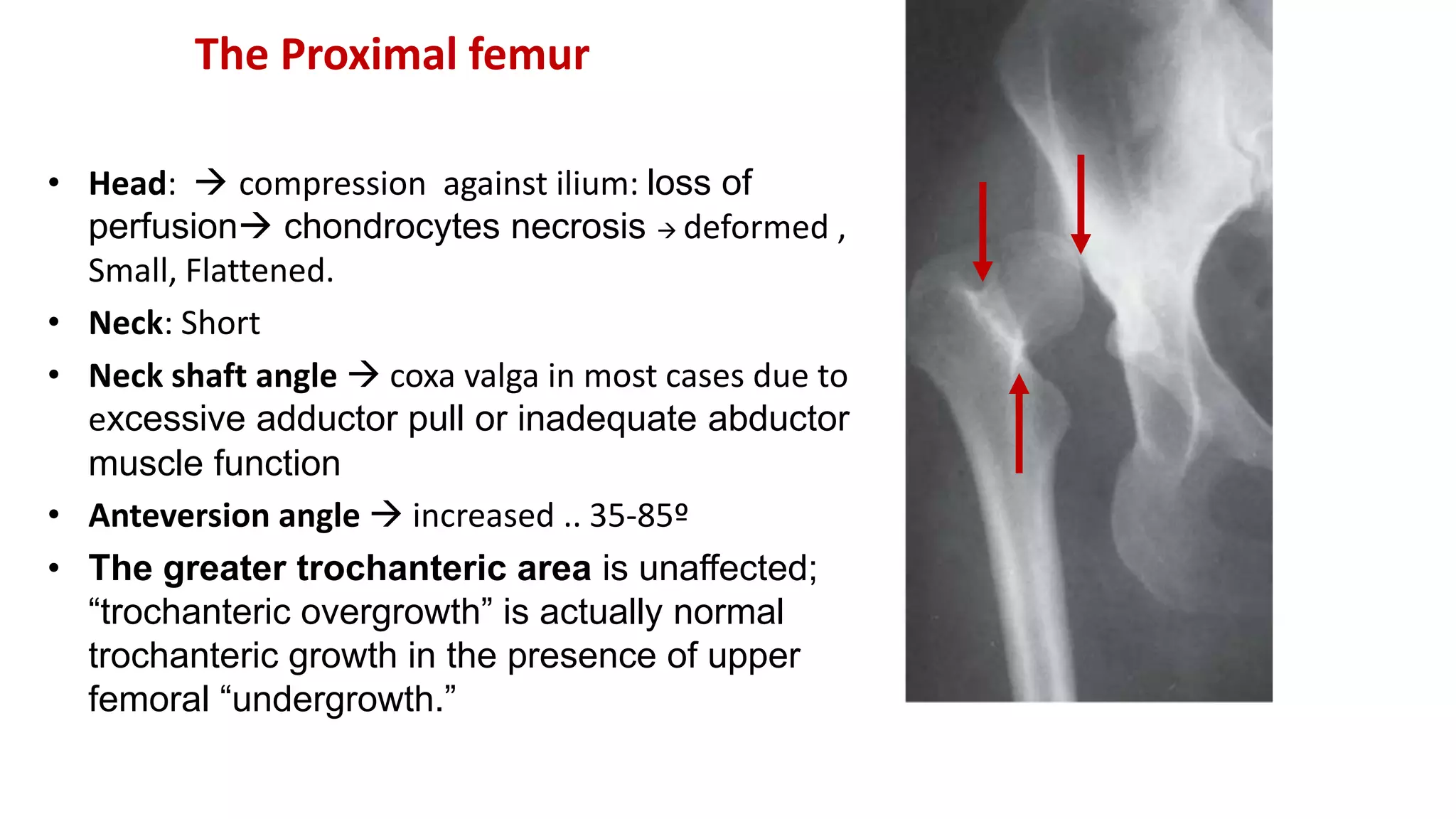
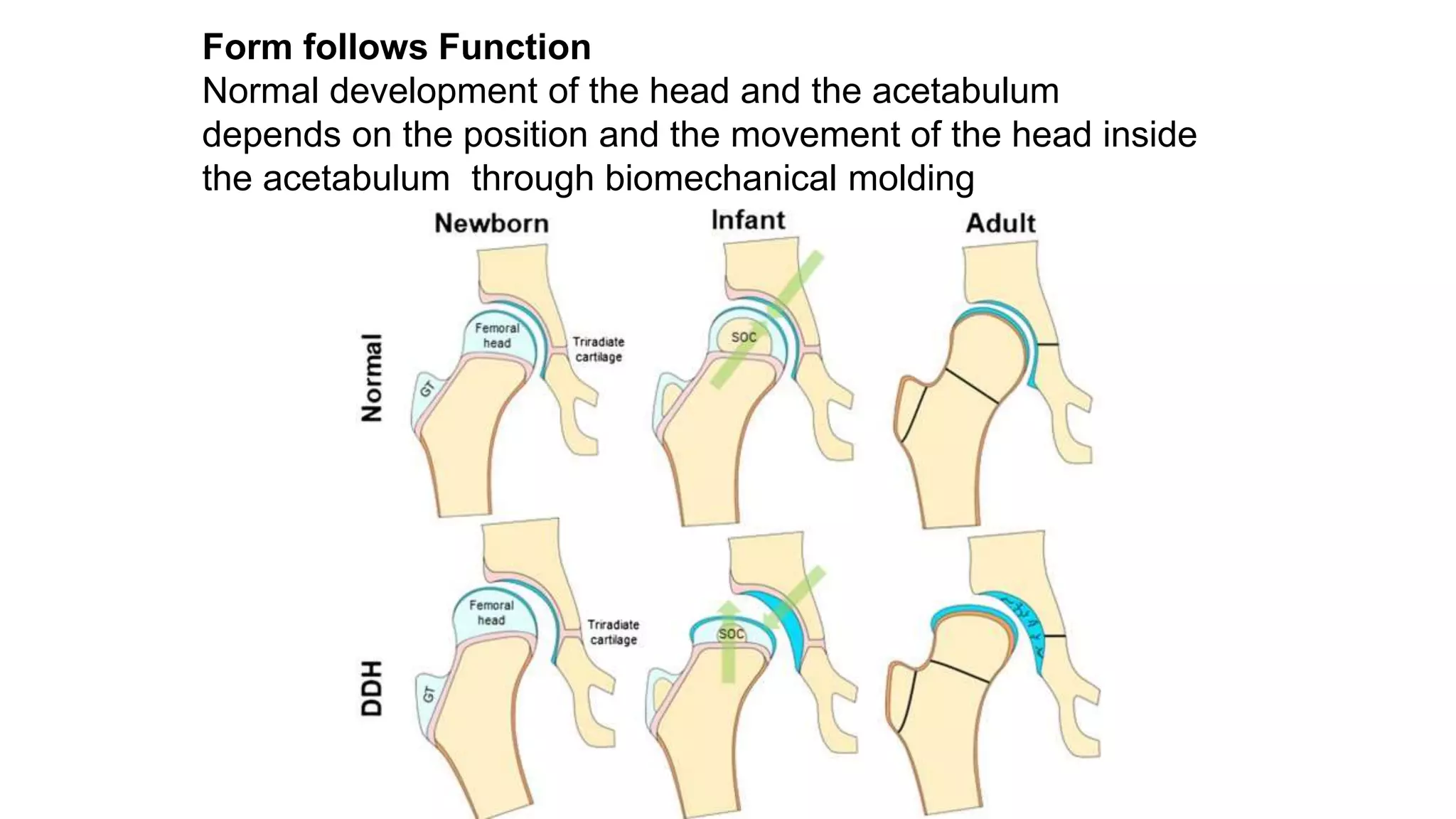
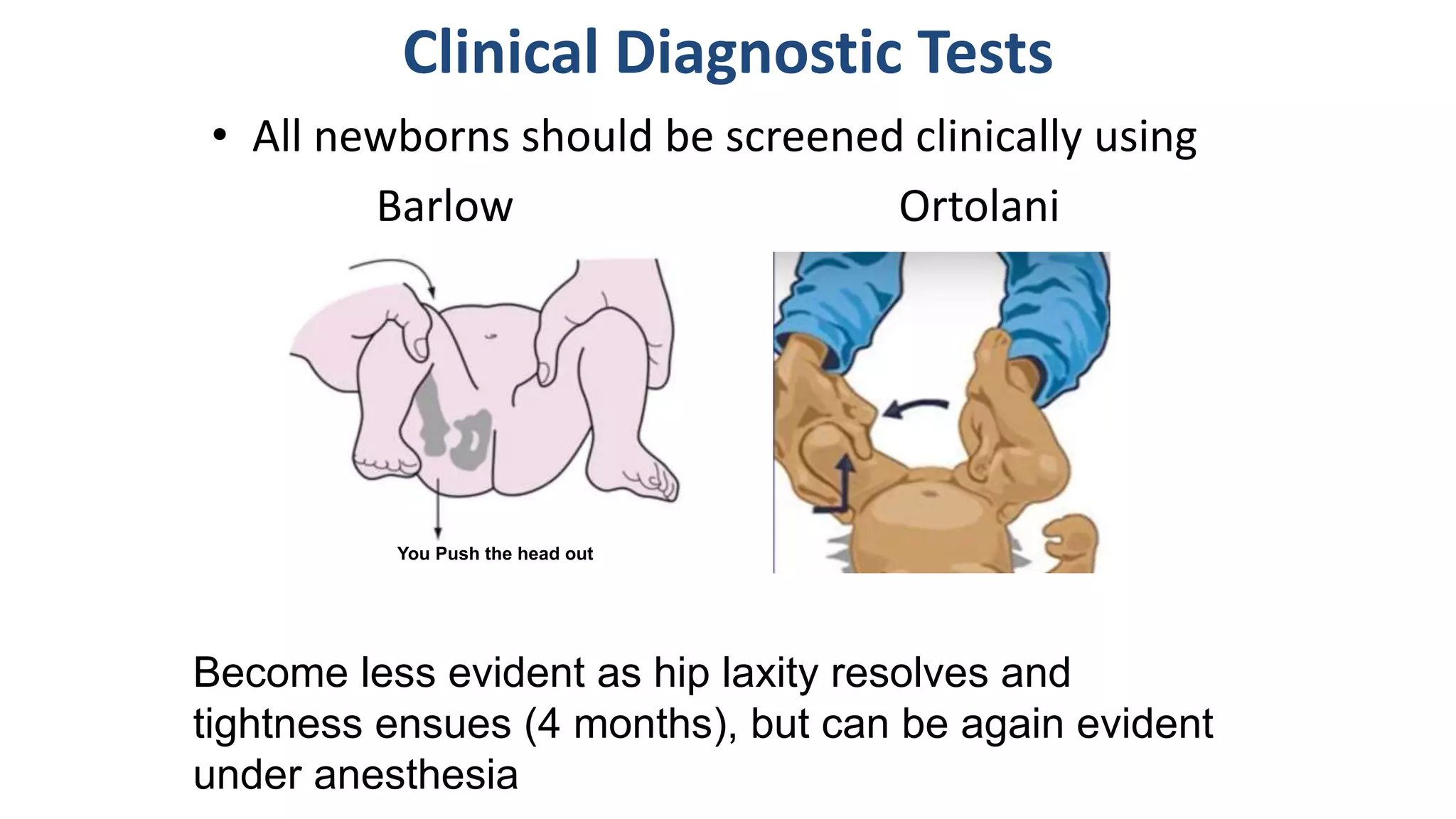
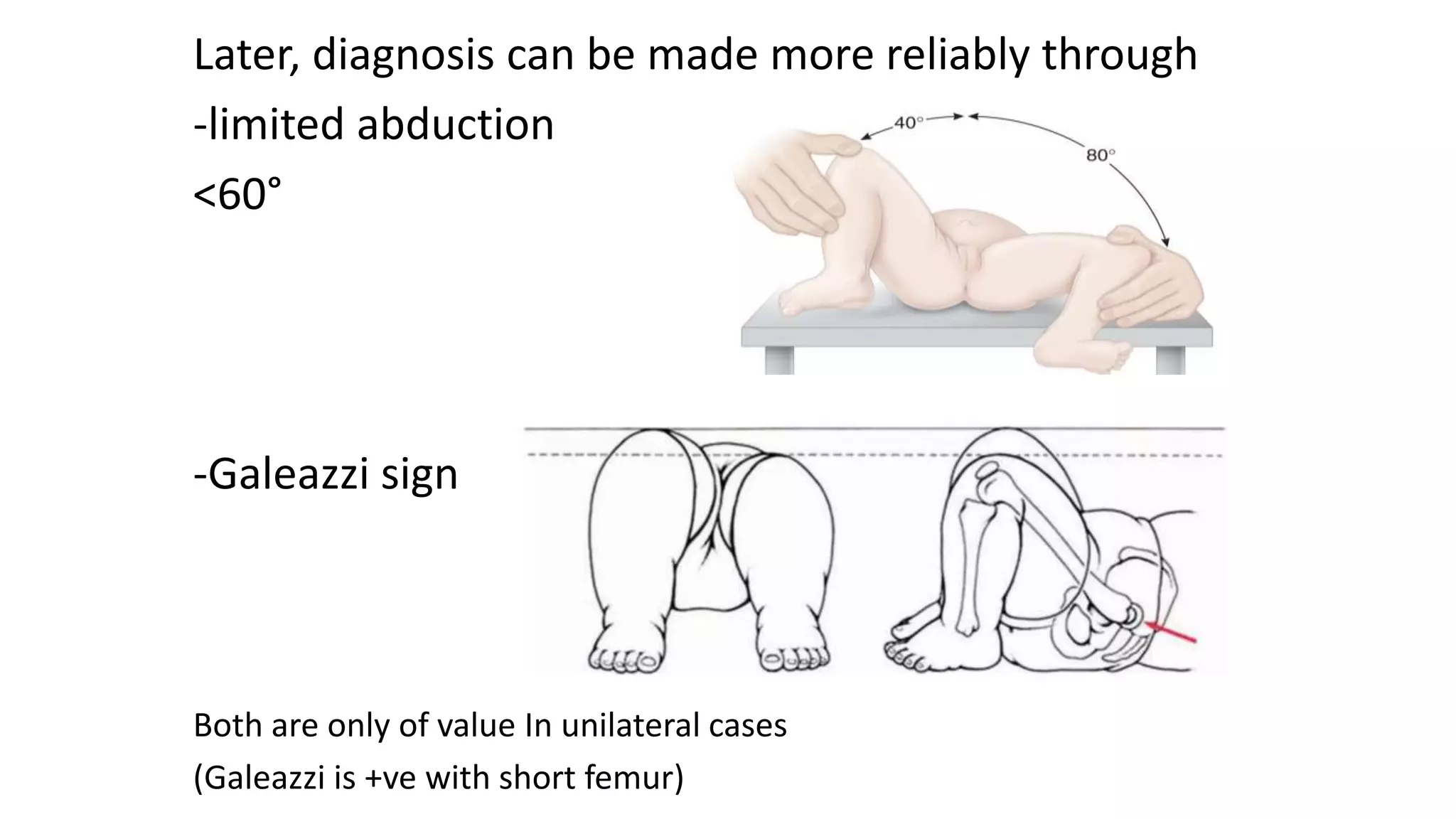
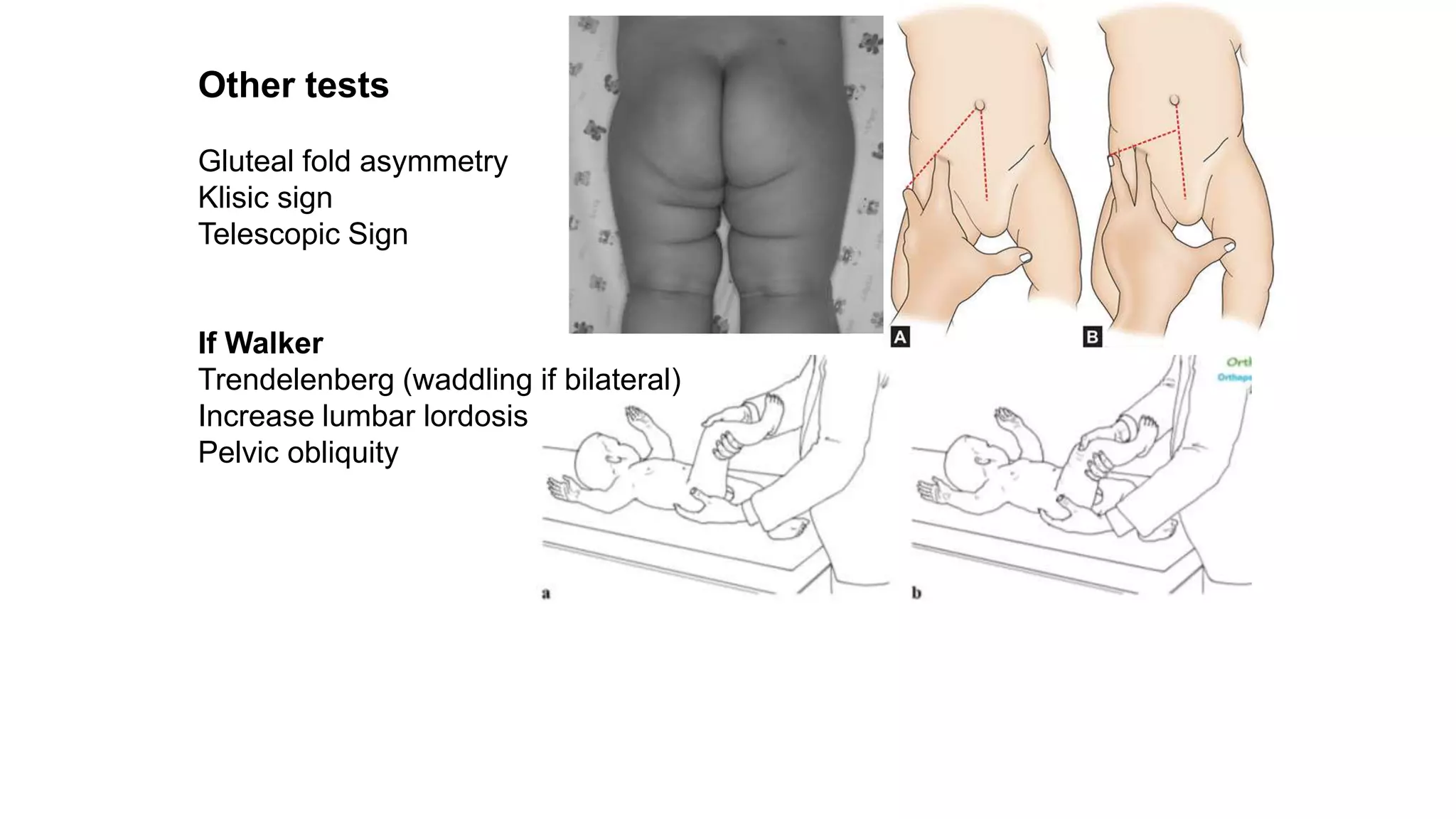
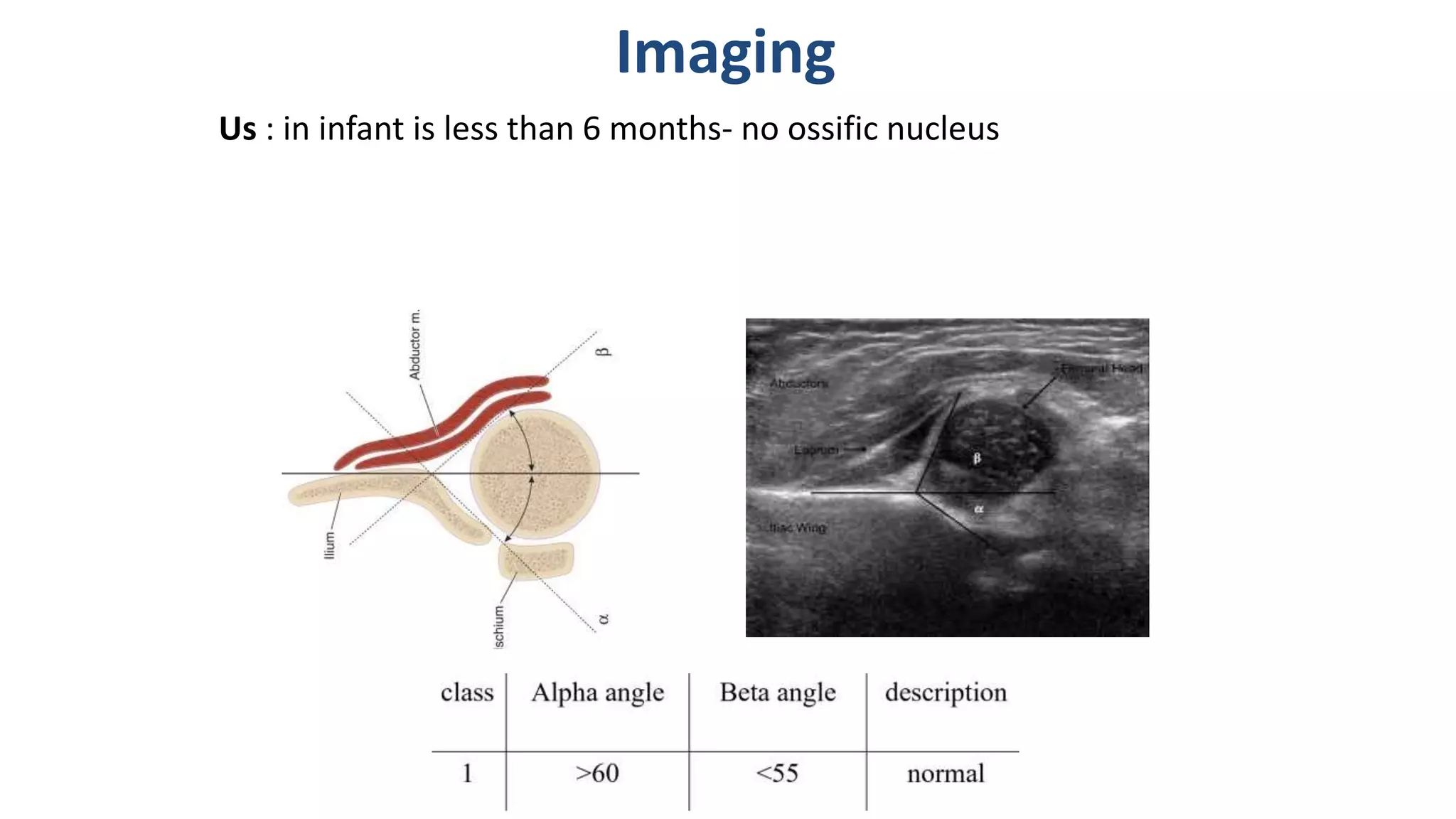
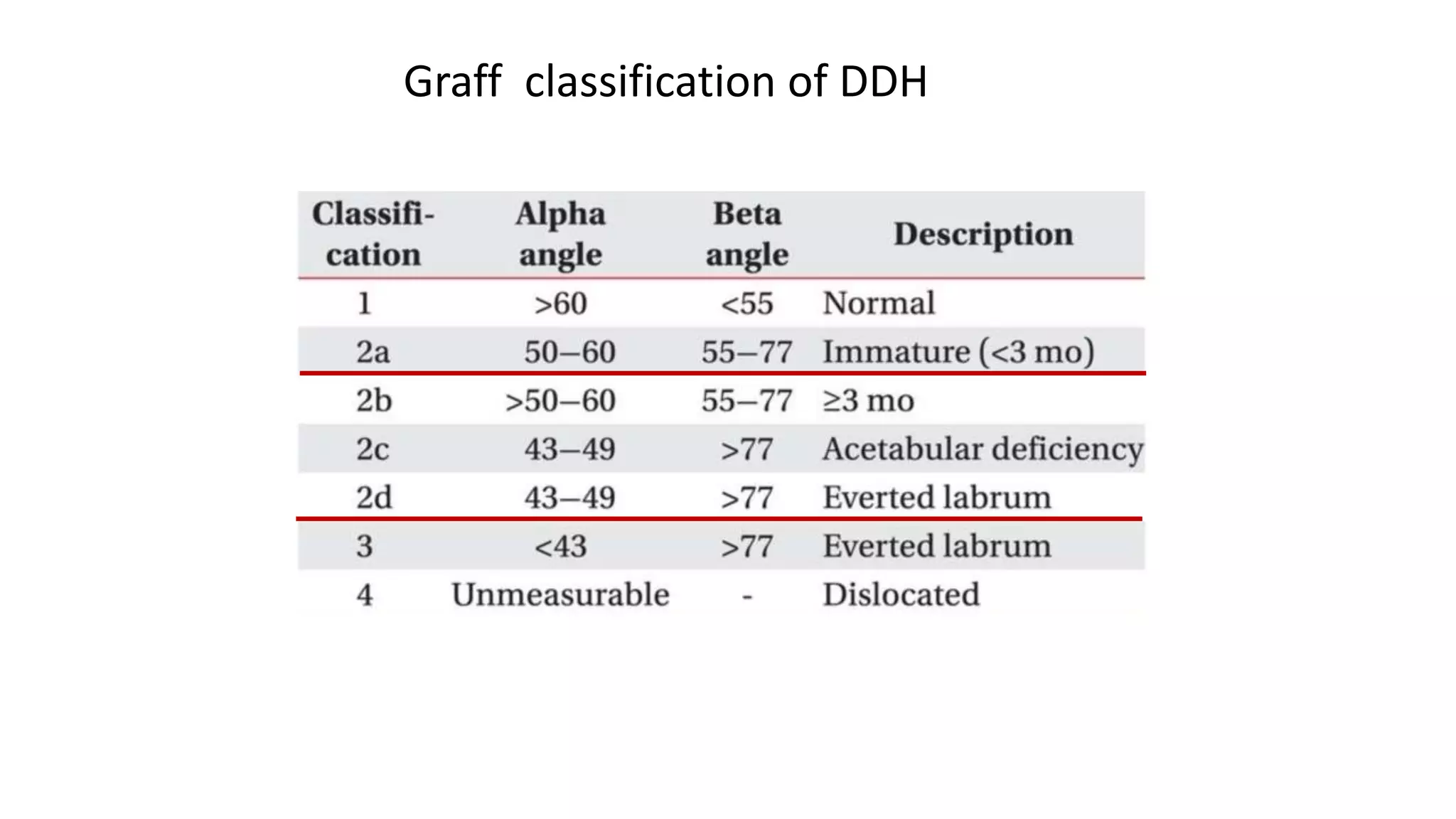
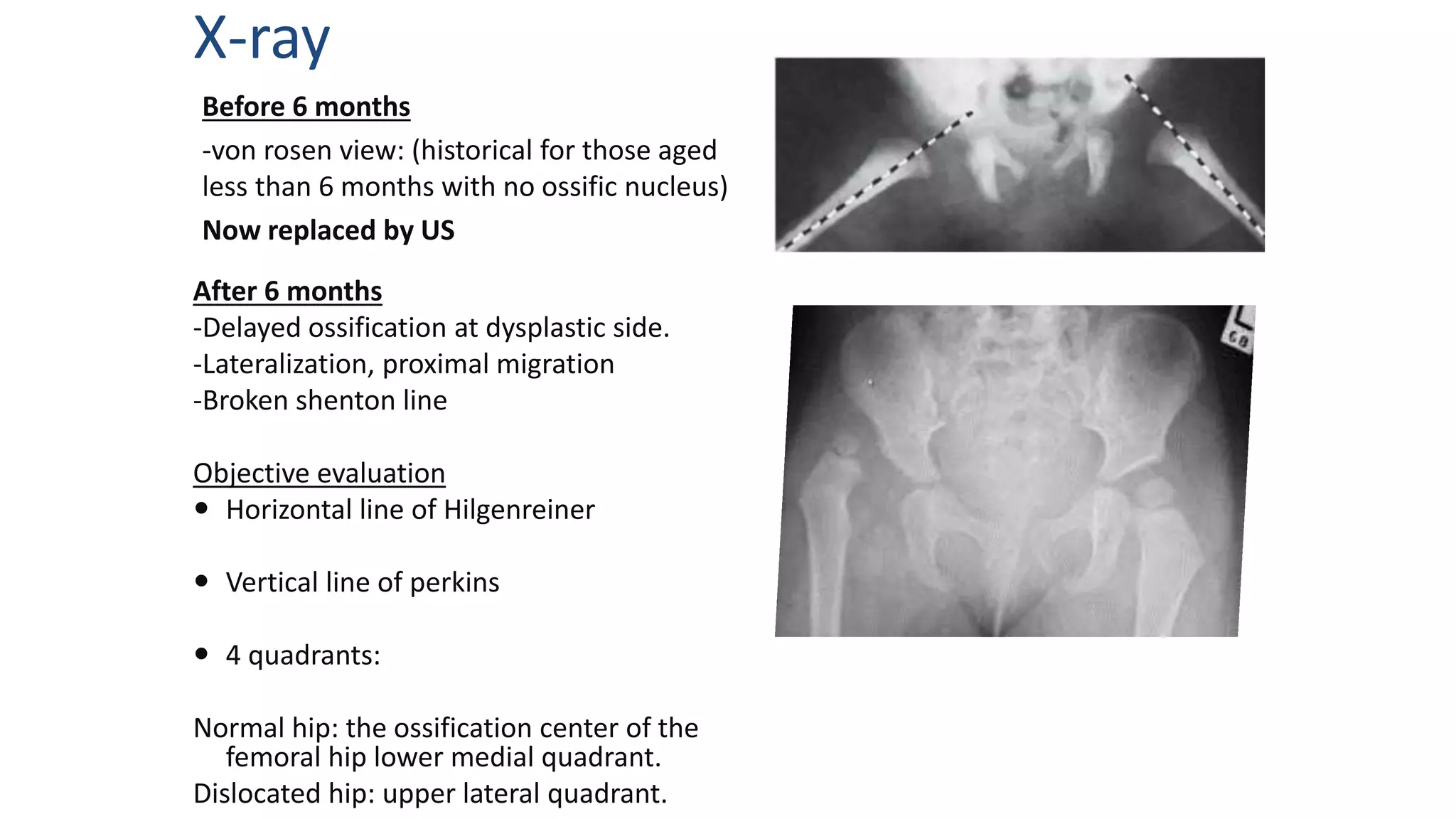
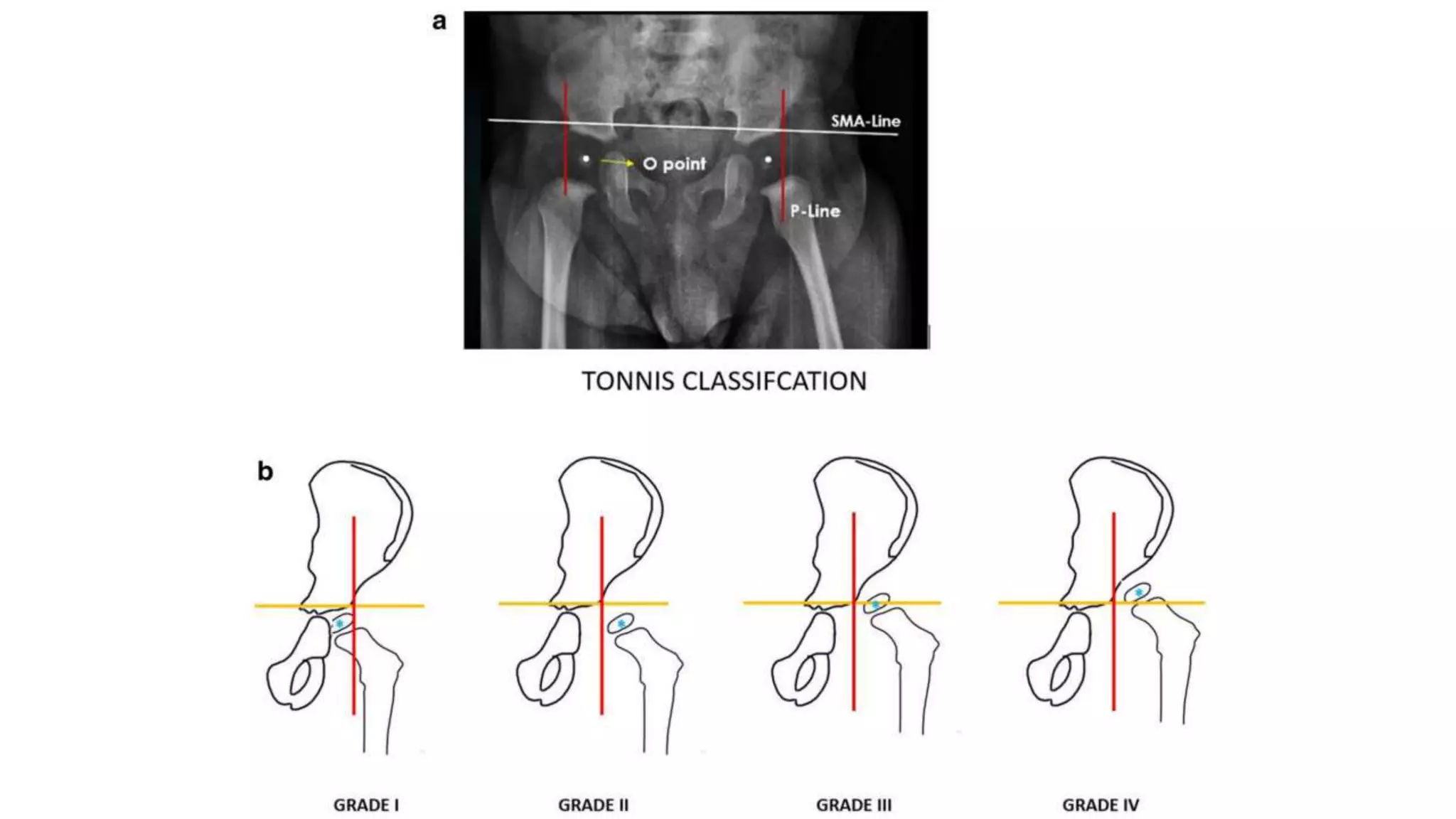
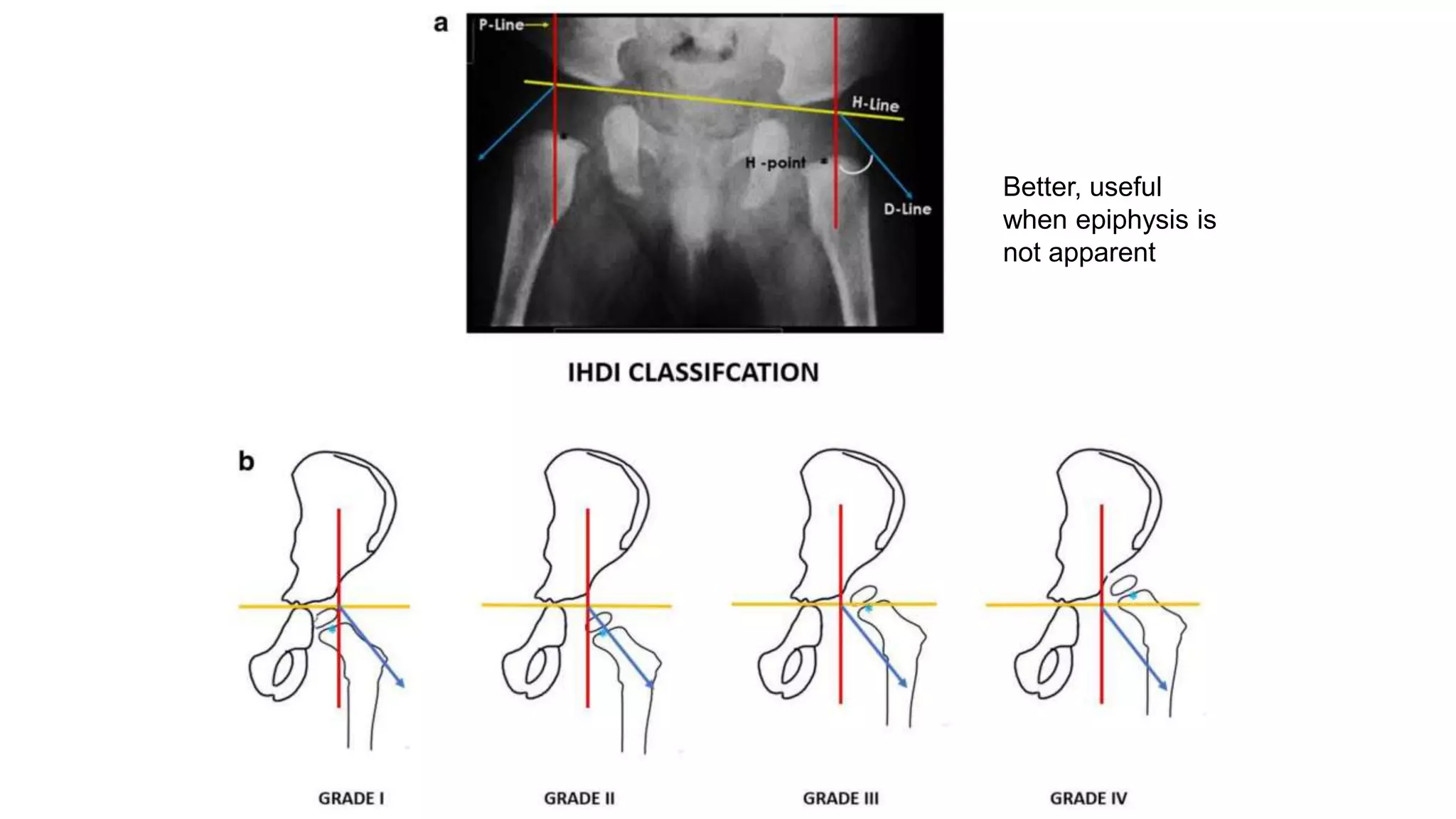
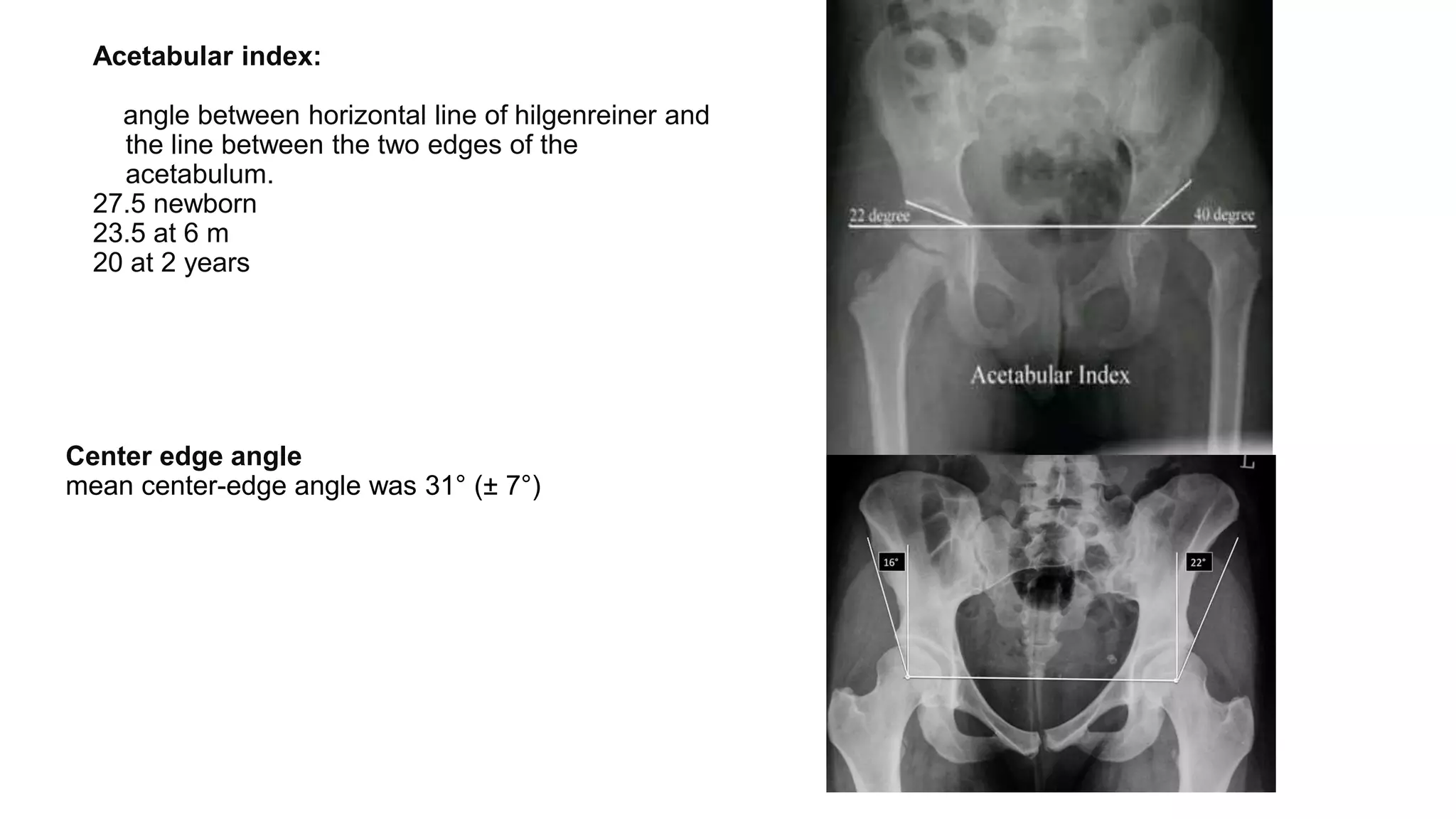
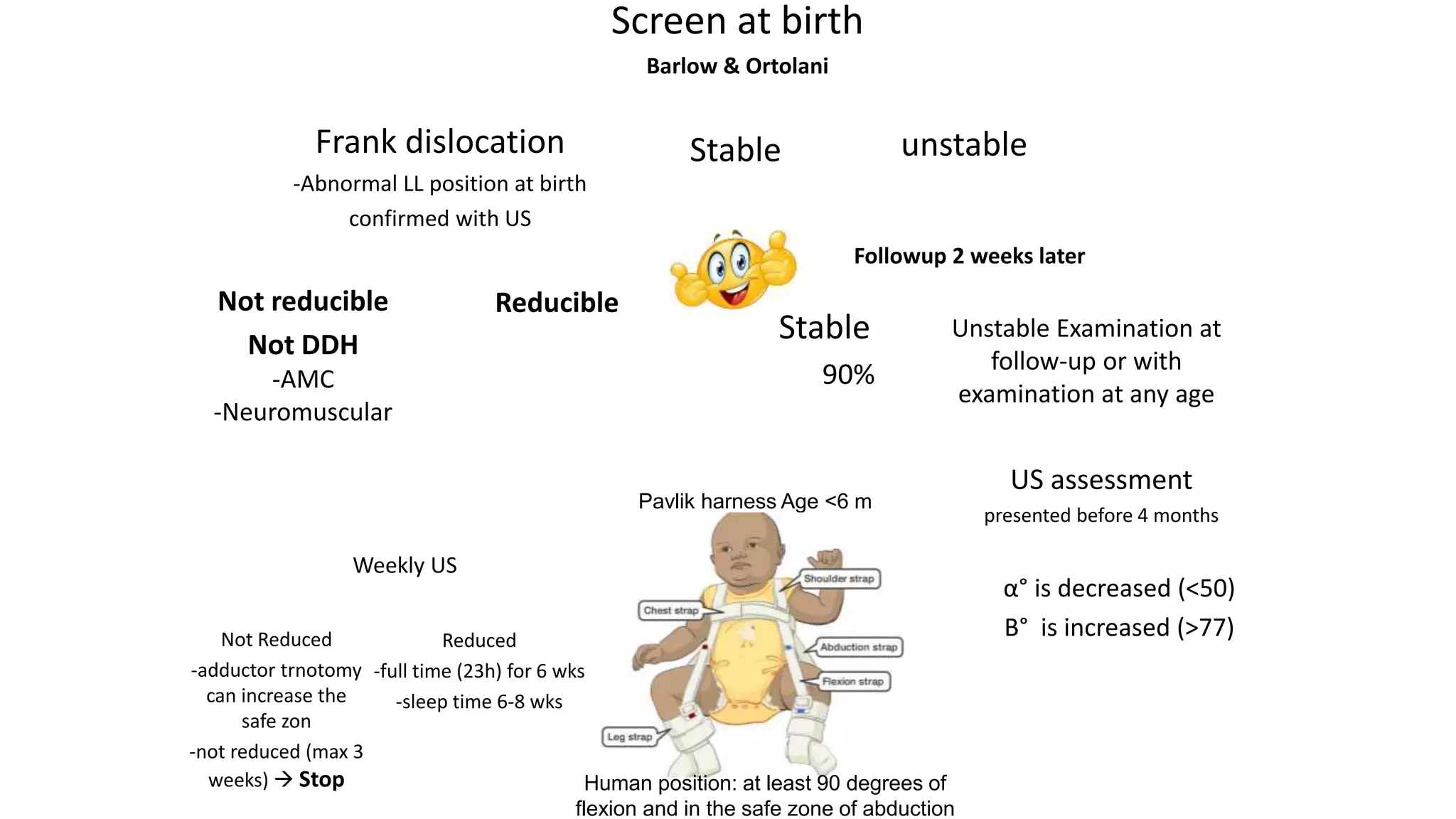
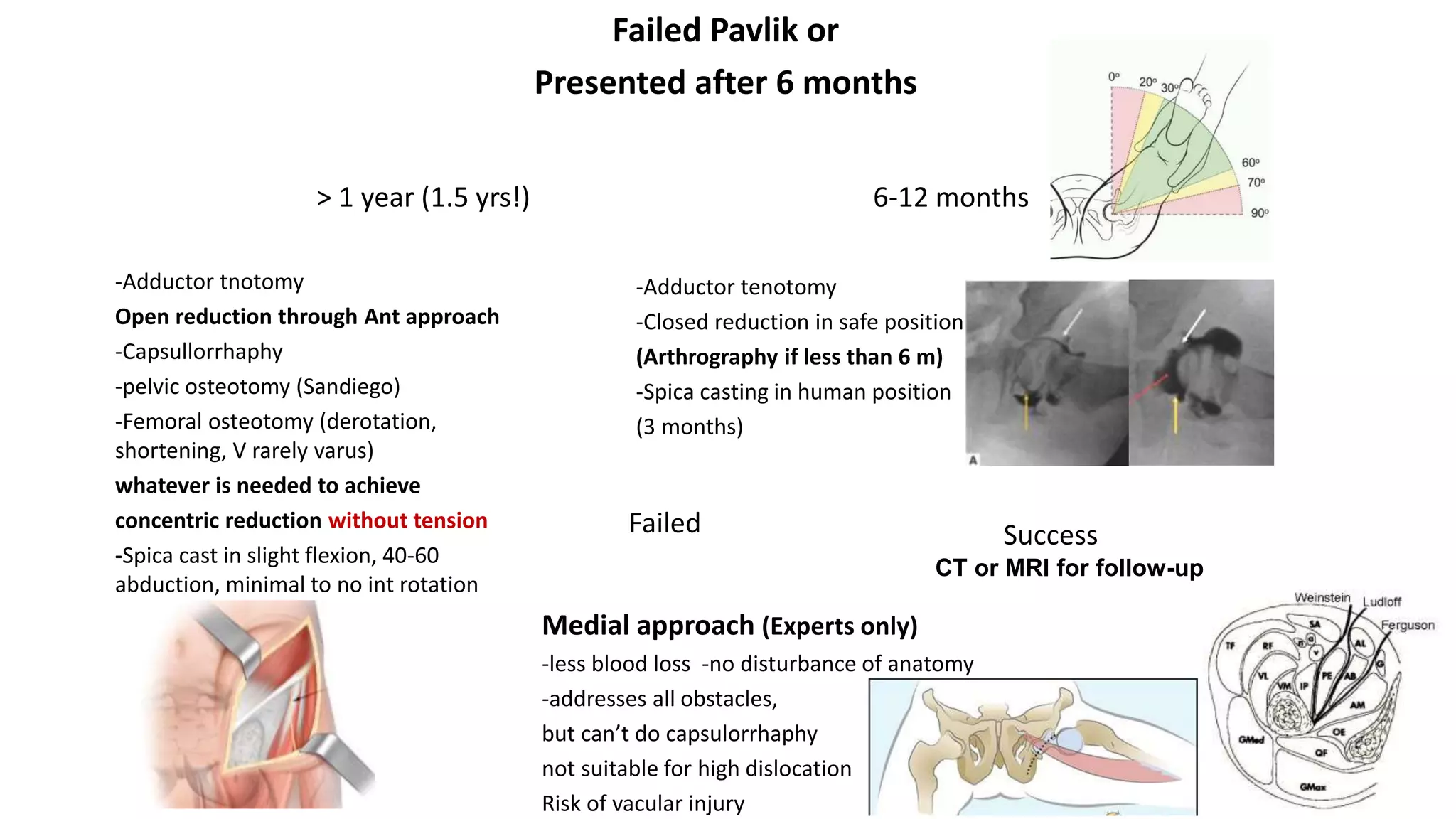
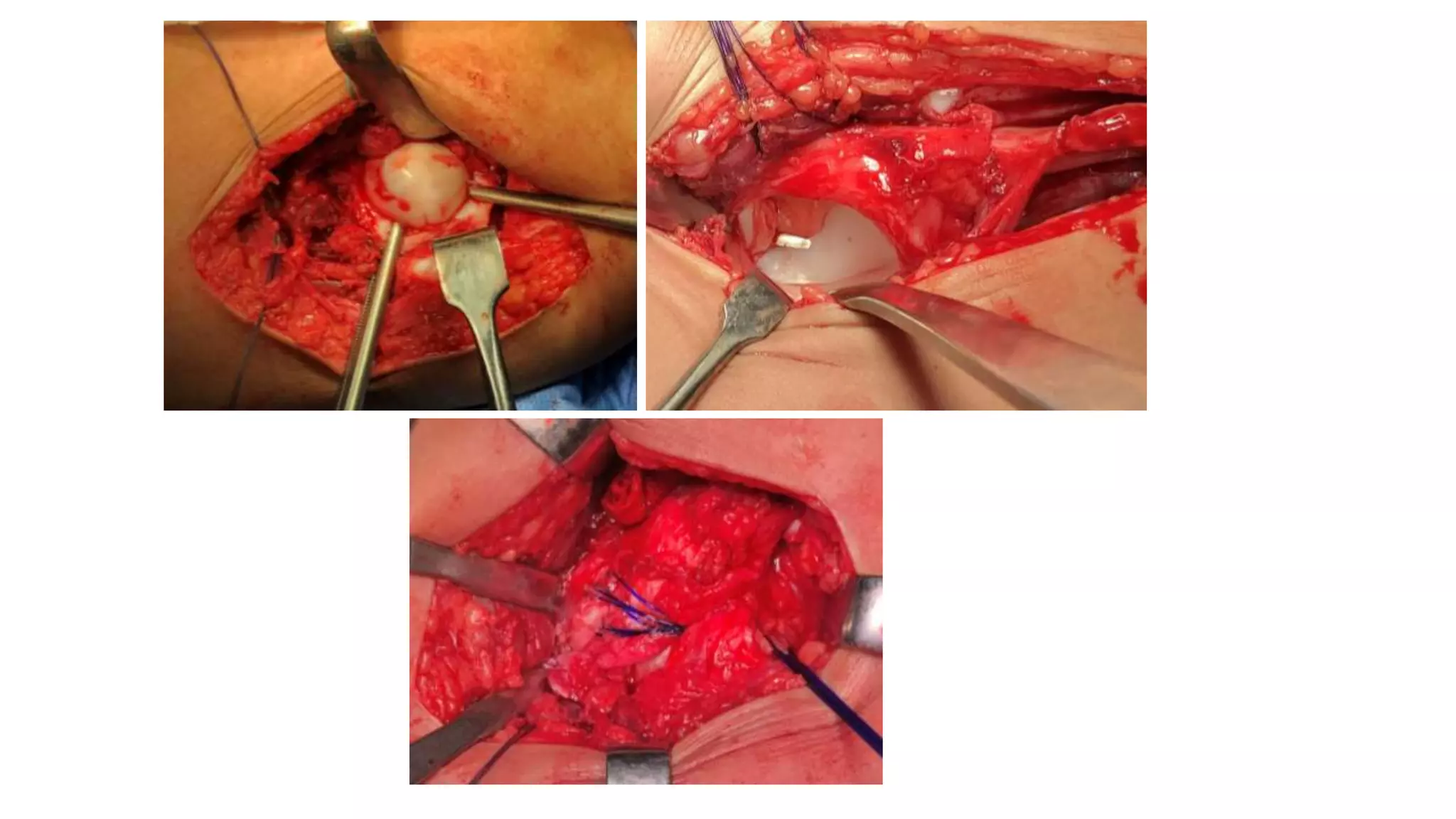
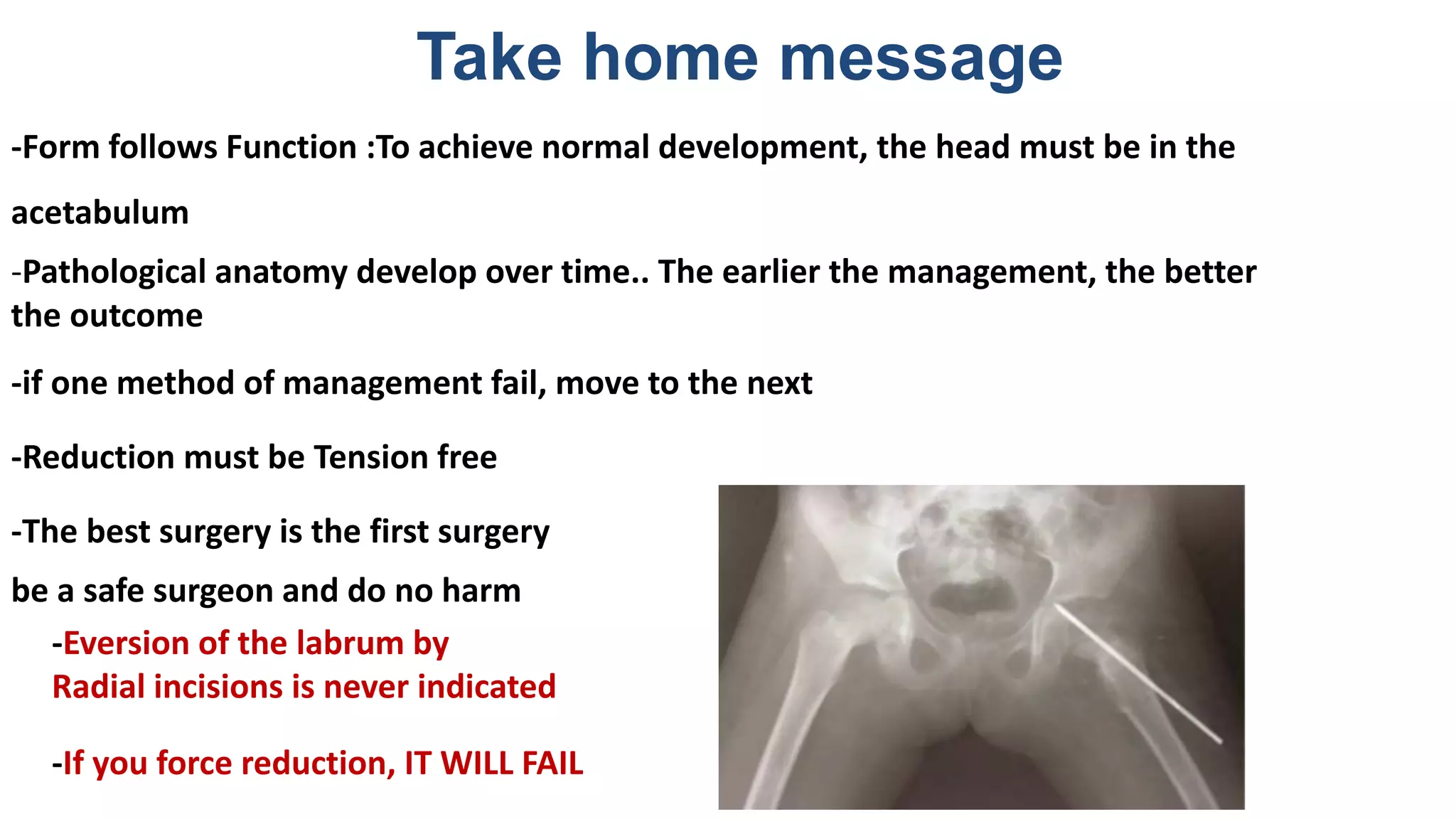
This document discusses developmental dysplasia of the hip (DDH), including its definition, incidence, causes, clinical tests for diagnosis, imaging techniques, and management approaches. DDH results from abnormal development of the hip joint and can range from instability to complete dislocation. Risk factors include female sex, breech positioning, and family history. Clinical exams include the Ortolani and Barlow tests. Ultrasound and x-rays are used for imaging. Treatment depends on age and severity, and may involve harnessing, casting, or surgery to achieve a concentric reduction without tension. The goal is normal development through positioning the femoral head in the acetabulum.