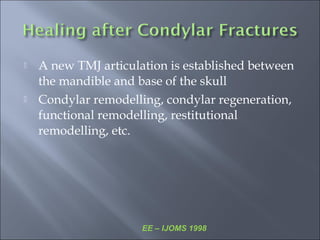
This document discusses fractures of the mandibular condyle. It notes that management principles and goals of treatment vary for these fractures compared to other mandibular fractures. The document covers the classification, clinical features, and management principles for condylar fractures. It discusses different surgical approaches for treating condylar fractures depending on the type and location of the fracture. Post-treatment, condylar remodeling can occur where a new temporomandibular joint articulation is established through bone adaptation processes.
![ M/F ratio – 2:1
Mean age – 29 yrs [4-76 yrs]
Most common cause of unilateral condylar # -
Males
RTA [40%]
Assaults [37%]
Females
RTA [42%]
Falls [36%]
Most common cause of bilateral condylar # -
Both M/F
RTA
Falls
Marker et al, BJOMS 2000, 348 pts](https://image.slidesharecdn.com/condylarfractures-ih-160522073431/85/Condylar-fractures-ih-8-320.jpg)
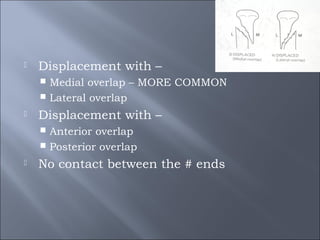
![ Non/Undisplaced [Fissure #]
Deviated – single angulation of the condylar
fragment to the distal mandibular segment
# ends remain in contact with no separarion or
overlap](https://image.slidesharecdn.com/condylarfractures-ih-160522073431/85/Condylar-fractures-ih-19-320.jpg)
![ Muscle attached with articular disc and have role in
displacement in condylar fracture
a) Lateral pterygoid b) Medial pterygoid c) Masseter d)
Temporalis
[Ans. a) Lateral pterygoid Ref. Pg. 117 B.D. Chaurasia]
The fibres run backwards and laterally and converge to be inserted
into :
1. The pterygoid fovea on the anterior surface of the neck of
mandible.
2. The anterior margin of the articular disc and capsule of the
temporomandibular joint
So its lateral pterygoid which is attached with articular disc and it
has role in displacement of condylar fractures.](https://image.slidesharecdn.com/condylarfractures-ih-160522073431/85/Condylar-fractures-ih-24-320.jpg)
![ Anterior displacement of fracture condyle is due to
a) Lateral pterygoid b) Buccinator c) Medial pterygoid d)
Temporalis
[Ans. (a) Ref-Neelima malik pg 351]
The muscle, under the influence of which, the superior
fragment of condyle, in a condylar neck # is displaced anteriorly
& medially is:
A. Medial pterygoid B. Lateral pterygoid C. Masseter D.
Temporalis
Ans. (B) Lateral pterygoid (Ref: Neelima Malik- 1st Ed/Pg 370)](https://image.slidesharecdn.com/condylarfractures-ih-160522073431/85/Condylar-fractures-ih-25-320.jpg)





![ Restoration of FORM and FUNCTION with
the use of SIMPLEST MEANS
[Walker, JOMS 1988 Discussion: open reduction of condylar # of the mandible in conjunction with
repair of discal injury: a preliminary report]](https://image.slidesharecdn.com/condylarfractures-ih-160522073431/85/Condylar-fractures-ih-40-320.jpg)
![ 8 wks
[JOMS, 1987 – Amaratunga etal; IJOMS, 2000 – Ed Ellis, G.
Throckmorton]
7-21 days –
Age of patient
Level of #
Degree of displacement
Presence of additional #](https://image.slidesharecdn.com/condylarfractures-ih-160522073431/85/Condylar-fractures-ih-42-320.jpg)
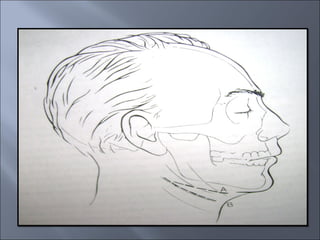
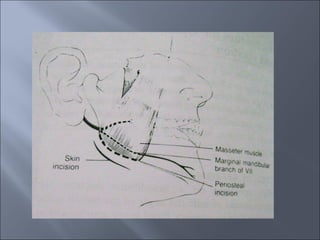
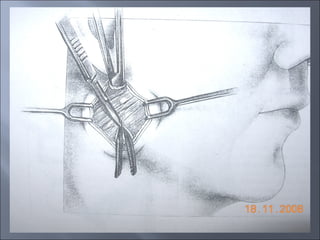
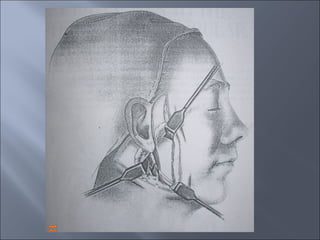
![ First described [1934] – Risdon
Dimensions
Site
Caution
Approach of choice for subcondylar fractures](https://image.slidesharecdn.com/condylarfractures-ih-160522073431/85/Condylar-fractures-ih-52-320.jpg)

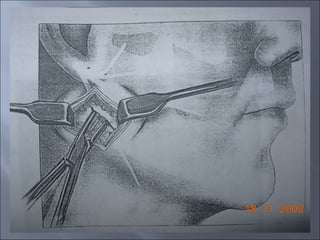
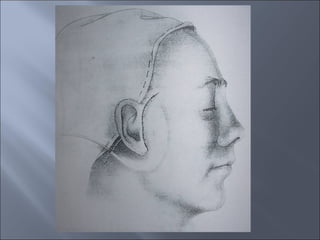
![ Modification of conventional submandibular
incision
Kruger [1990] discussed it](https://image.slidesharecdn.com/condylarfractures-ih-160522073431/85/Condylar-fractures-ih-55-320.jpg)
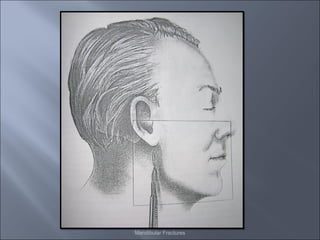
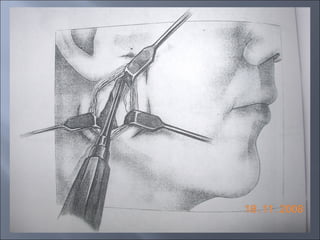
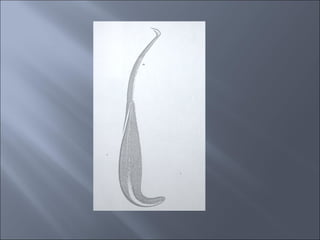
![ Steinhauser [1964] first described it
Lacher – 1st
only for low subcondylar #
Later, all extracapsular #
Technique
Incision
Dissection
Pitayama’s intraoral technique](https://image.slidesharecdn.com/condylarfractures-ih-160522073431/85/Condylar-fractures-ih-74-320.jpg)
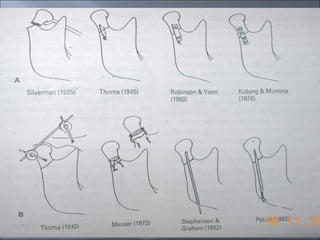
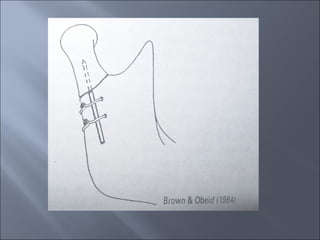
![ Only reduction without fixation
[Rees, Weinberg, 1983 OOO]
Suture ligatures
[Upton L]
External fixation
Use of K-wires
[Stephenson and Graham, 1952 and Lund and Takenoshita]
Osteosynthesis Wires – transosseous wiring
[Henny, Thoma, Messer, Tasanen and Lamberg]
Axial Anchorage screws
[Petzel and Kernel]
Rigid plates and screws](https://image.slidesharecdn.com/condylarfractures-ih-160522073431/85/Condylar-fractures-ih-76-320.jpg)
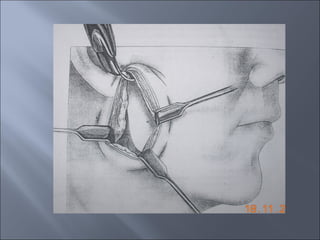
![ Use of moule pin
[Stewart and Bowerman, 1991]
Use of extracoporeal fixation
[Mikkonen et al, Ellis and Dean, Boyne]
Use of monocortical plate fixation
[Ellis E.](https://image.slidesharecdn.com/condylarfractures-ih-160522073431/85/Condylar-fractures-ih-77-320.jpg)
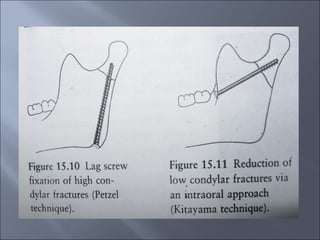
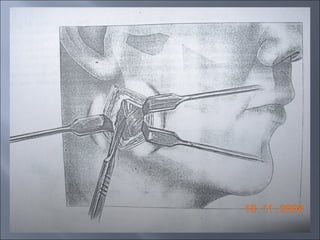
![ Use of artery forceps
Use of K-wire
Use of moule pin [BJOMS 1991, Stewart and
Bowerman]
Extracorpreal fixation
Use of Petzel’ technique](https://image.slidesharecdn.com/condylarfractures-ih-160522073431/85/Condylar-fractures-ih-81-320.jpg)