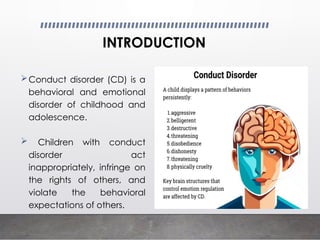
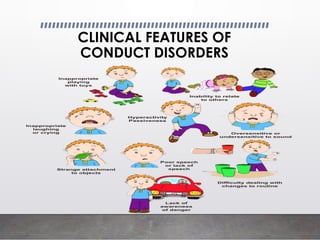
Conduct disorder (CD) is a childhood psychiatric issue characterized by aggressive behavior, violation of societal norms, and antisocial acts. It can be classified based on severity and age of onset, with risk factors including familial, social, and environmental influences. Treatment approaches involve early intervention, skill training for parents, cognitive behavioral therapy, and consistent communication between caregivers and educators.