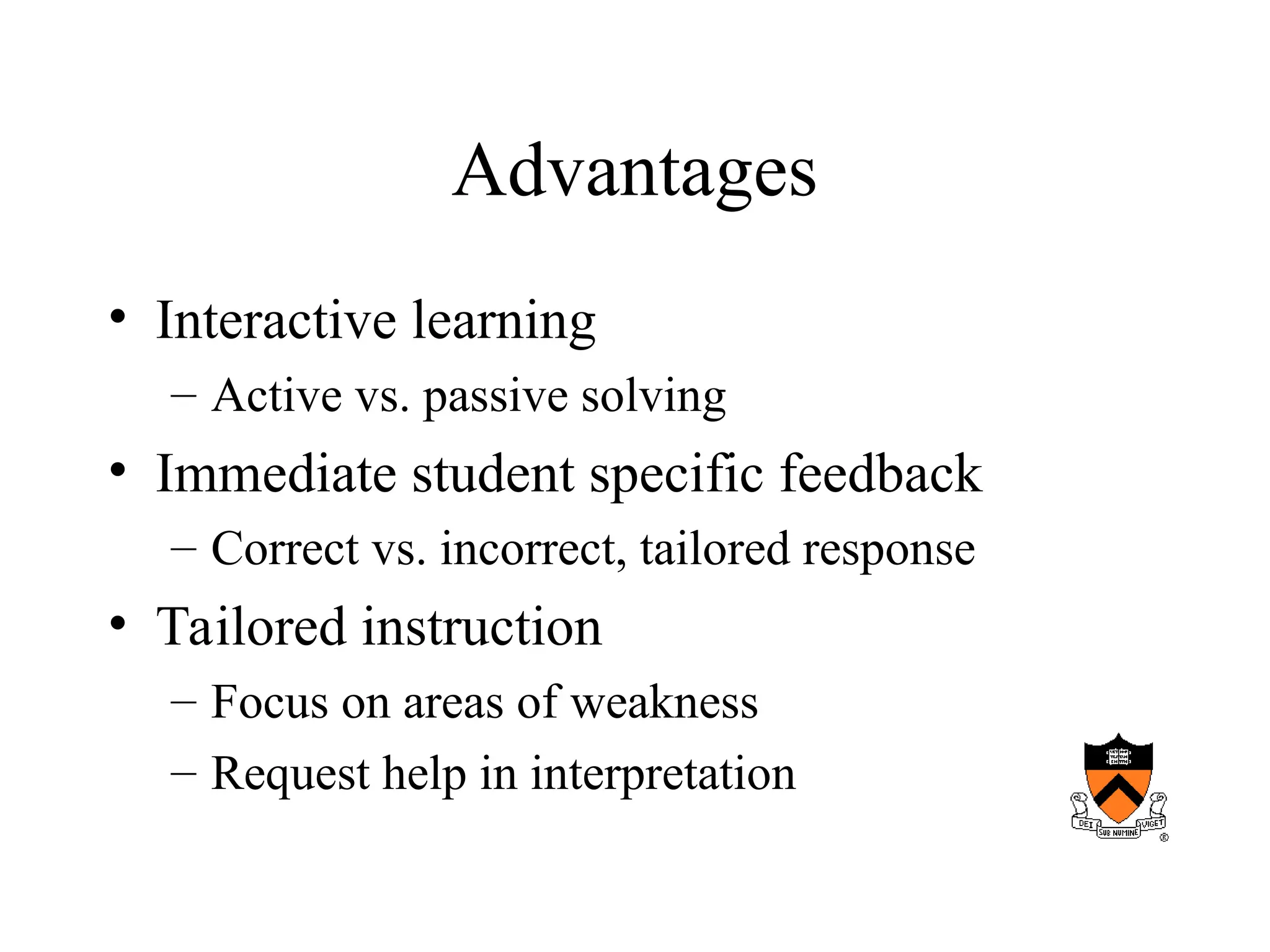
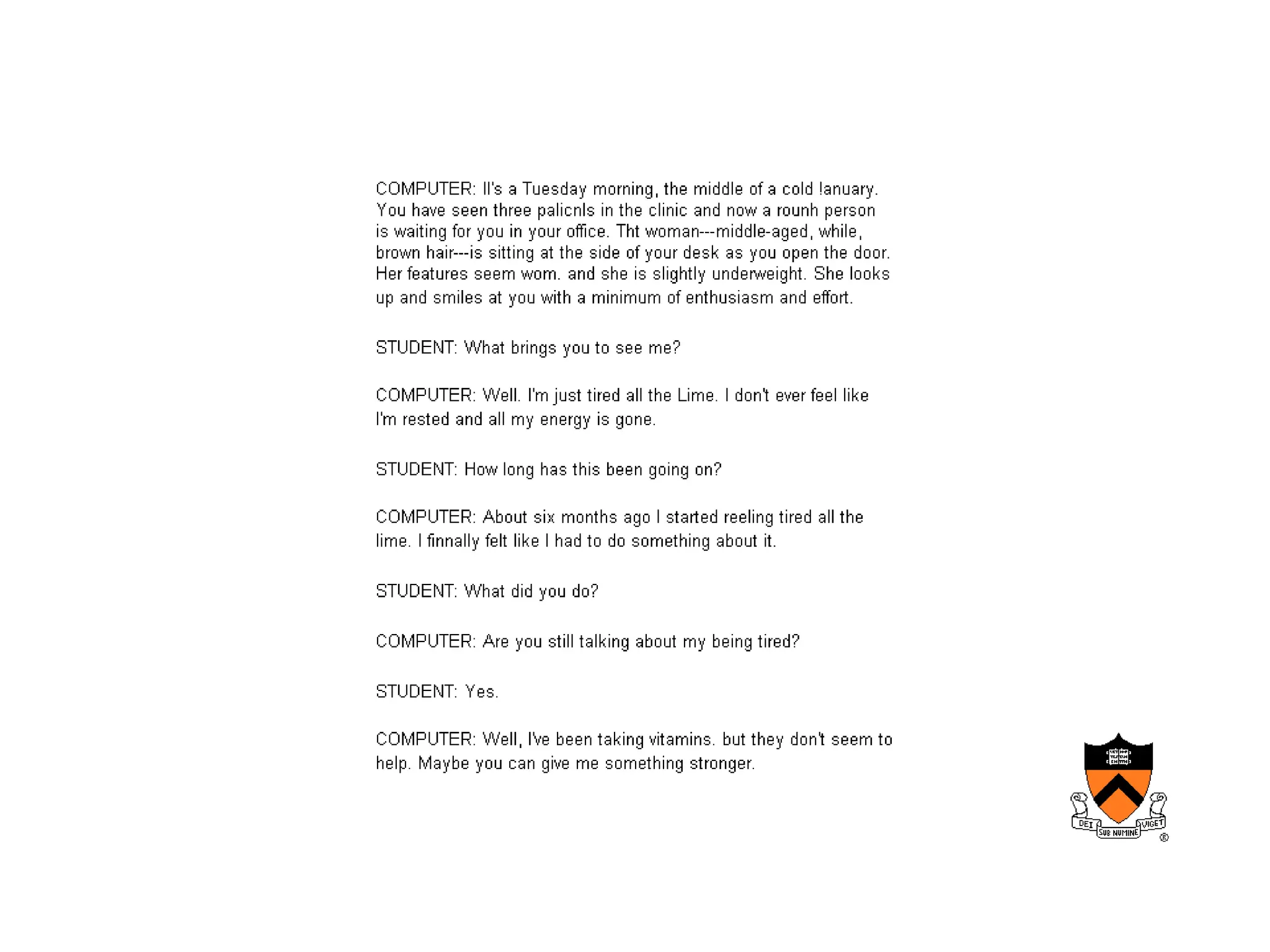
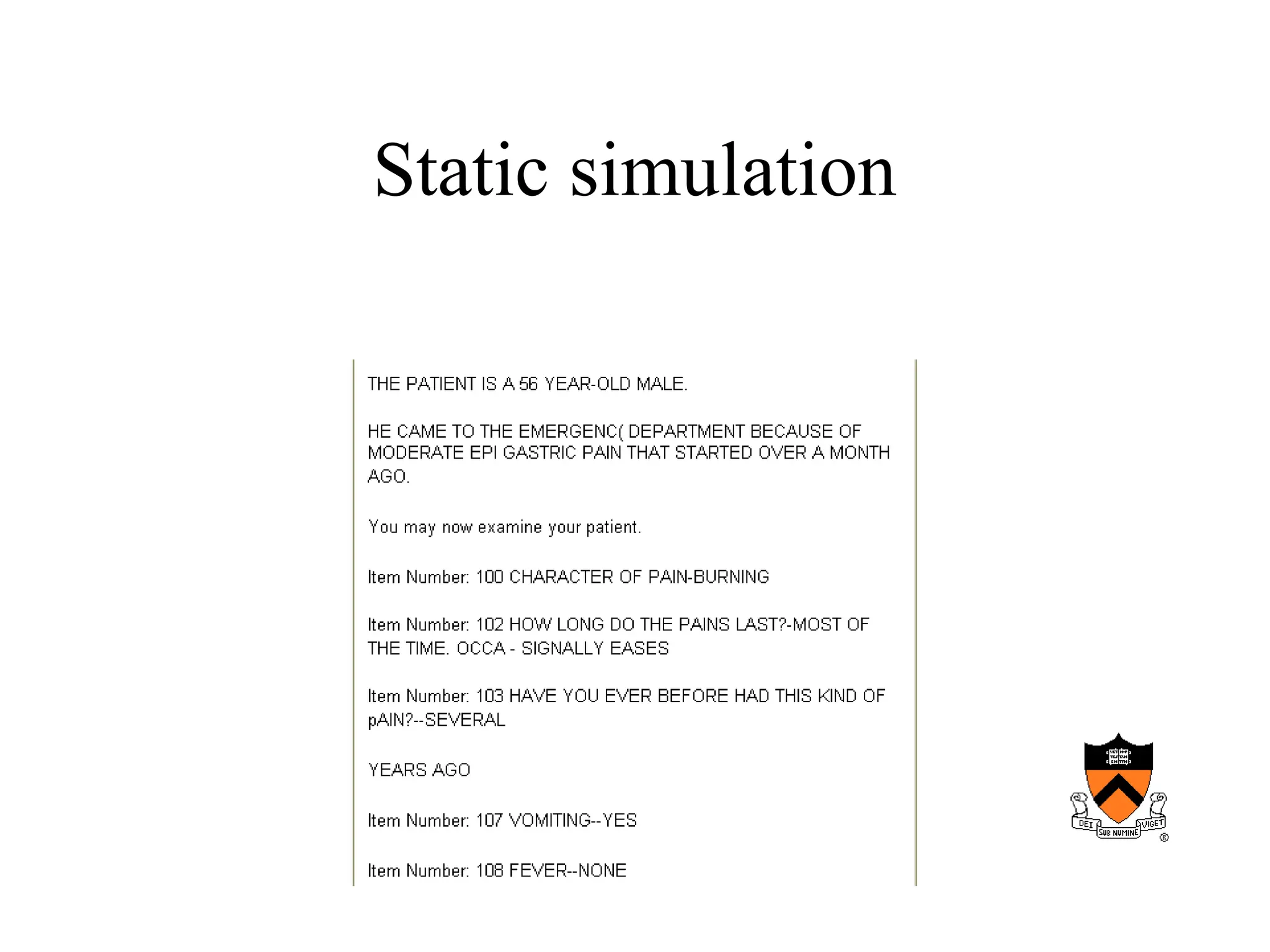
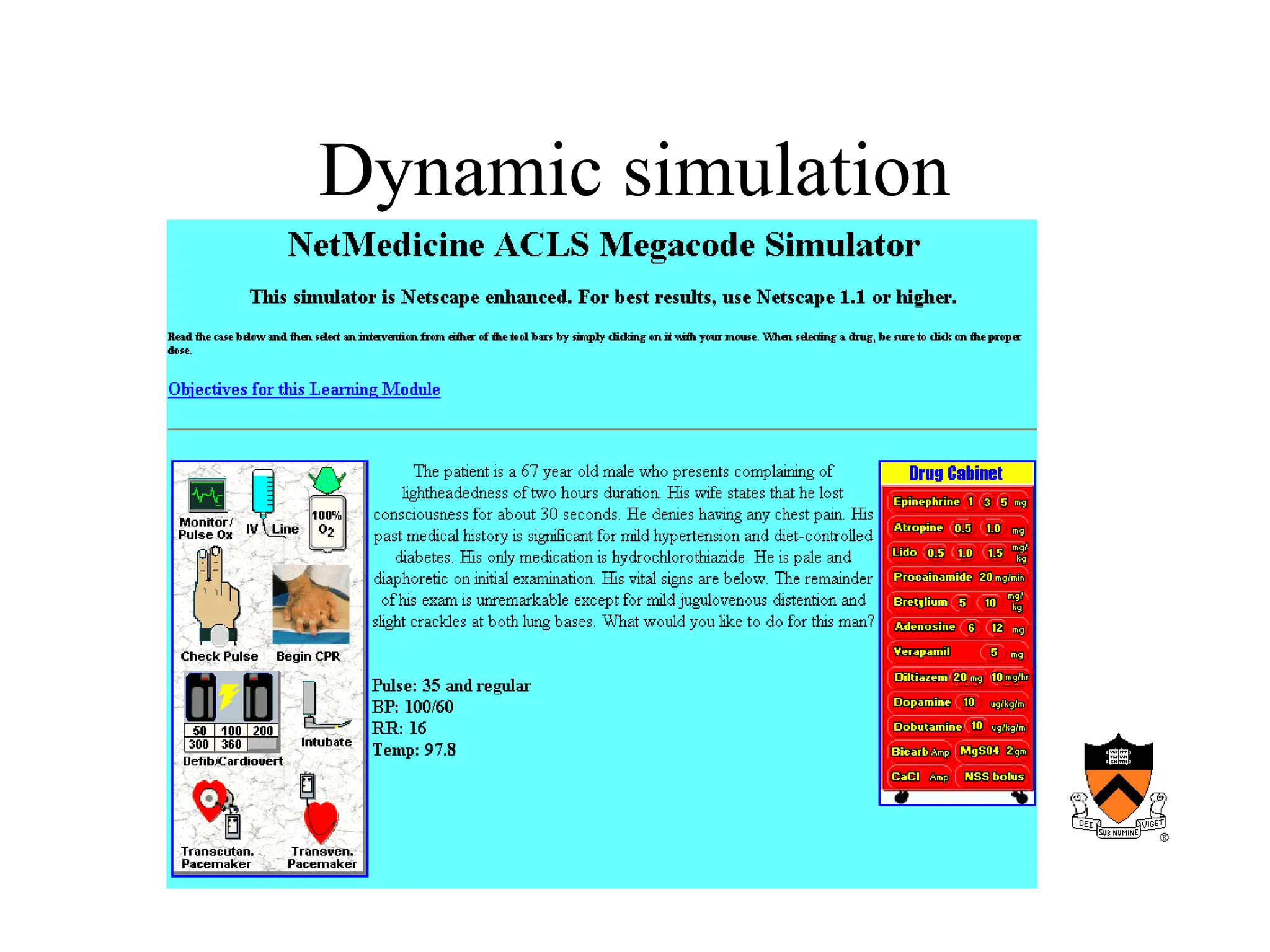
The document discusses the significant role of computers in medical education, emphasizing their ability to enhance traditional teaching methods and encourage active learning. It highlights the advantages of computer-assisted instruction, including immediate feedback and tailored learning experiences, while also addressing weaknesses of traditional education such as reliance on memorization. The content covers the evolution of computer-based education and its future potentials, including challenges like cost and immaturity of authoring tools.