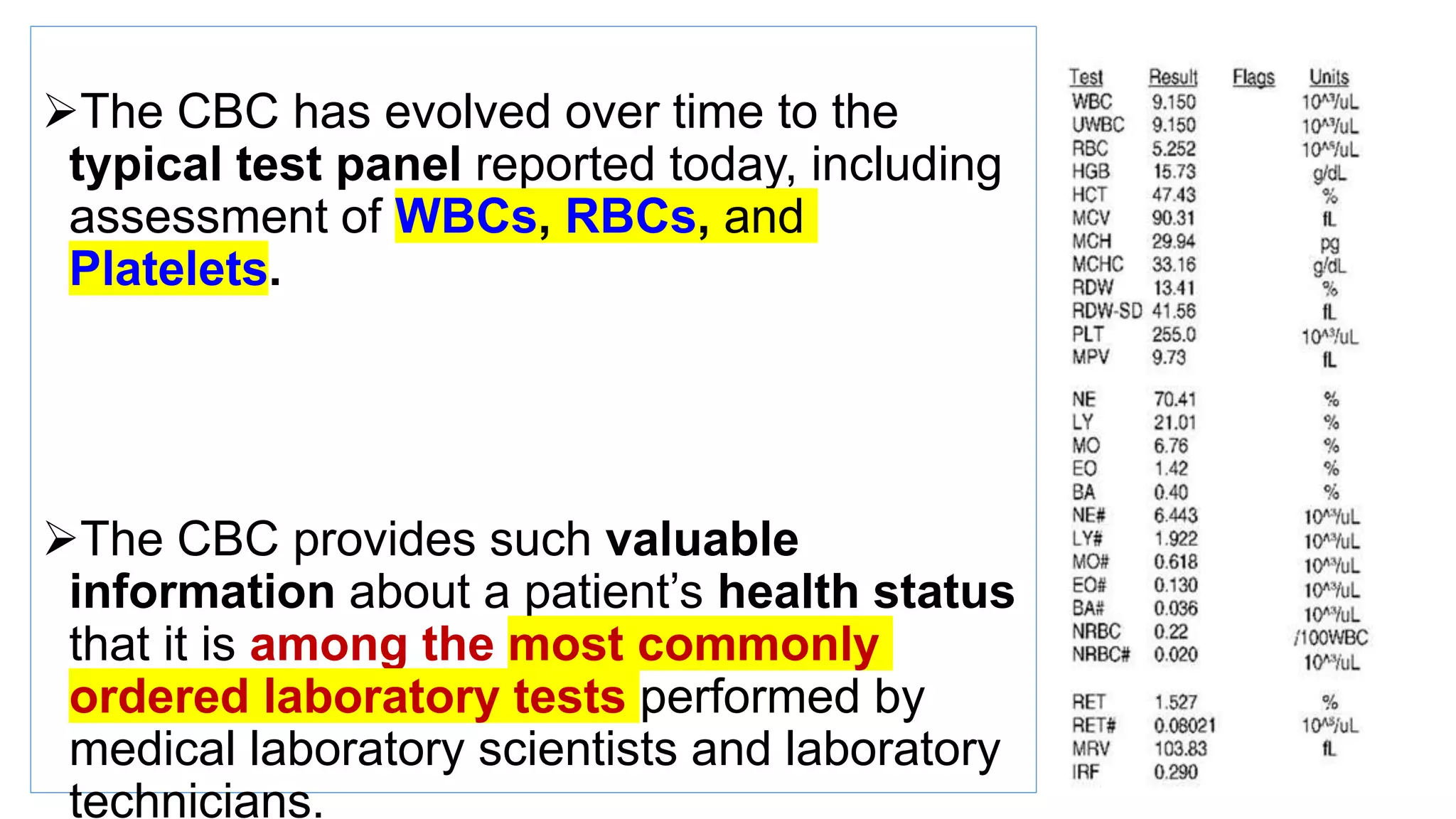
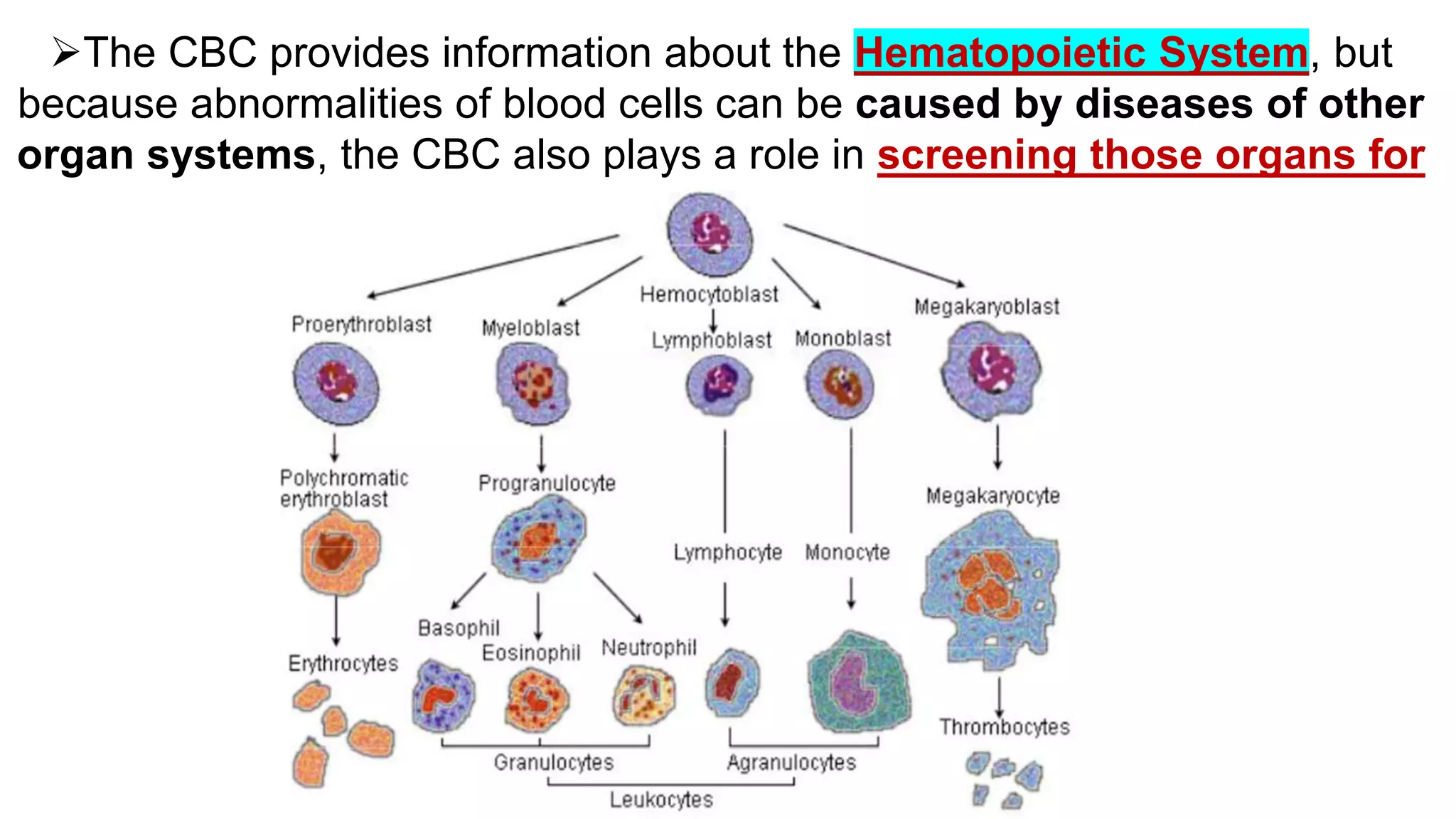
The document provides information on interpreting a complete blood count (CBC). It discusses the parameters assessed in a CBC including white blood cells (WBCs), red blood cells (RBCs), and platelets. It outlines the systematic approach to interpreting each component, beginning with ensuring an accurate WBC count and comparing to reference intervals. The WBC differential analysis examines relative and absolute counts as well as morphology. RBC analysis examines hemoglobin, mean corpuscular volume, mean corpuscular hemoglobin concentration, red cell distribution width, and morphology. Platelet analysis examines count, mean platelet volume, and morphology. The document also discusses interpreting elevations or decreases in these values.