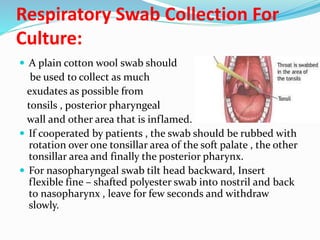
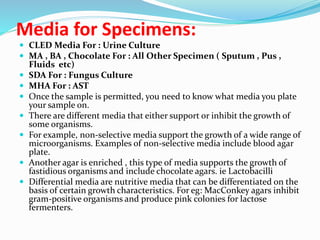
This document provides information about specimen collection and processing in a medical laboratory. It discusses key steps like collecting specimens aseptically, proper labeling and documentation, safe transport, and timely analysis. Common specimens include blood, urine, sputum, and swabs from various body sites. The document outlines procedures for collecting different types of specimens, appropriate containers, transport and storage conditions. It emphasizes the importance of aseptic technique and quality control.