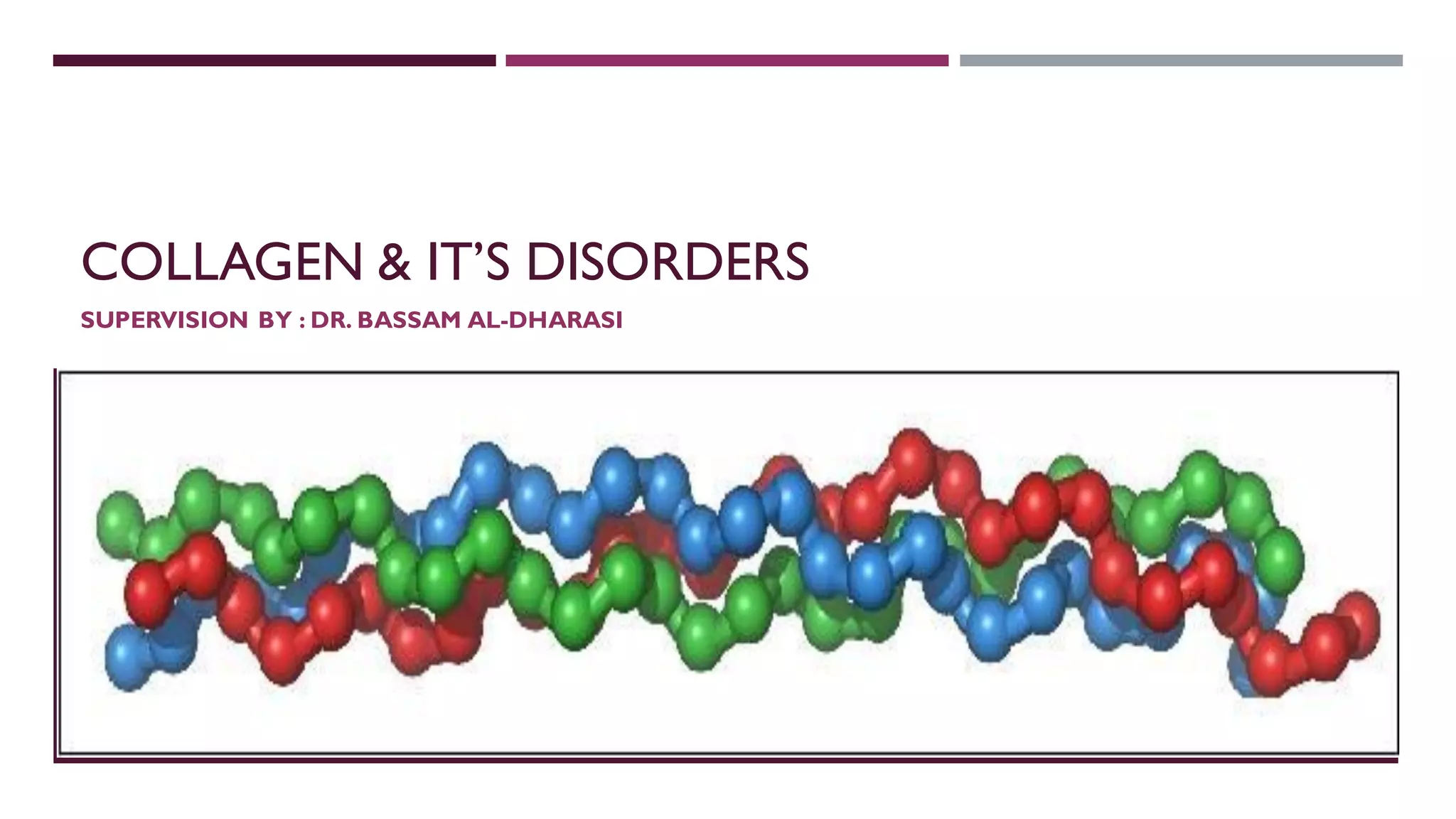
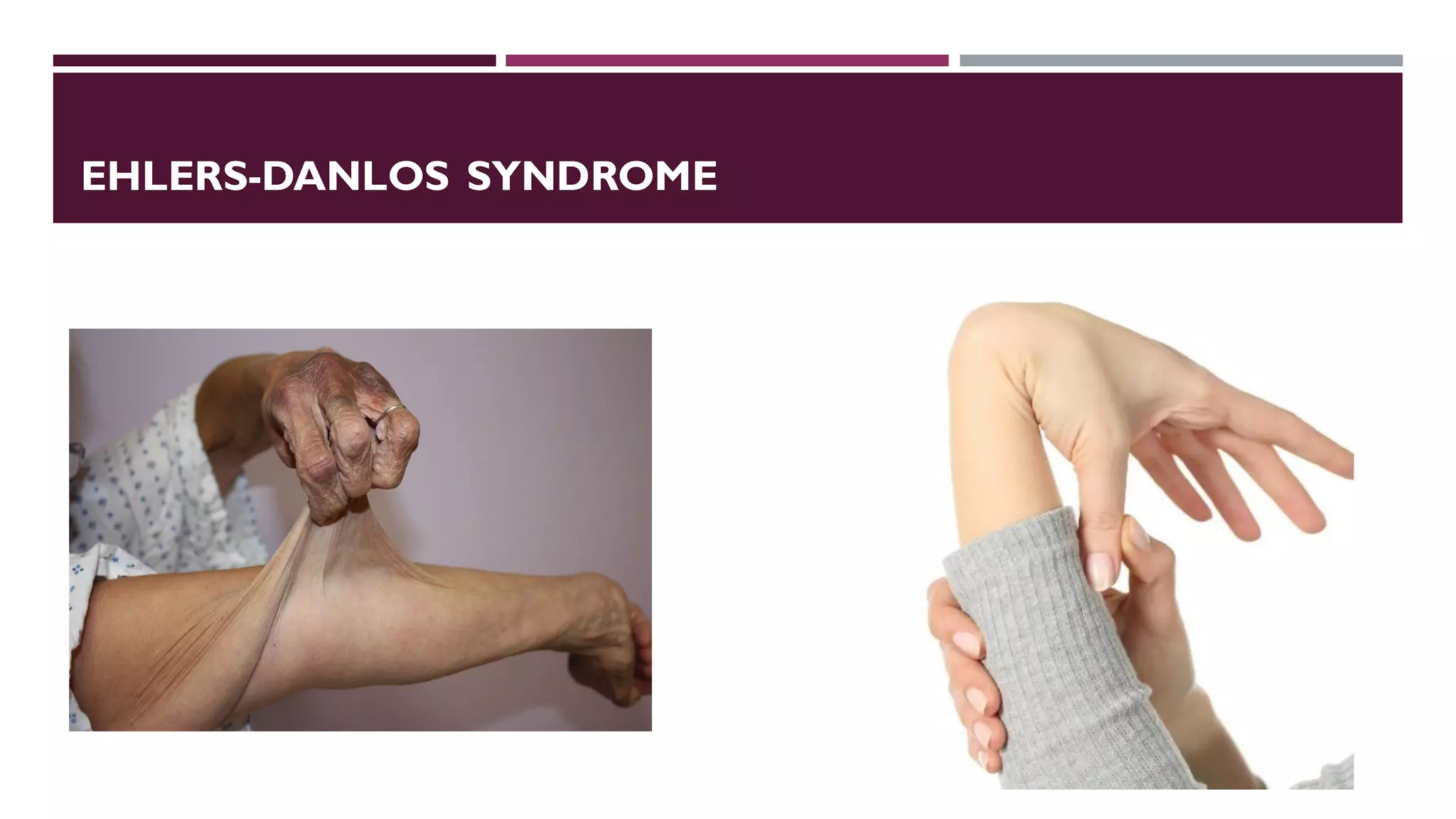
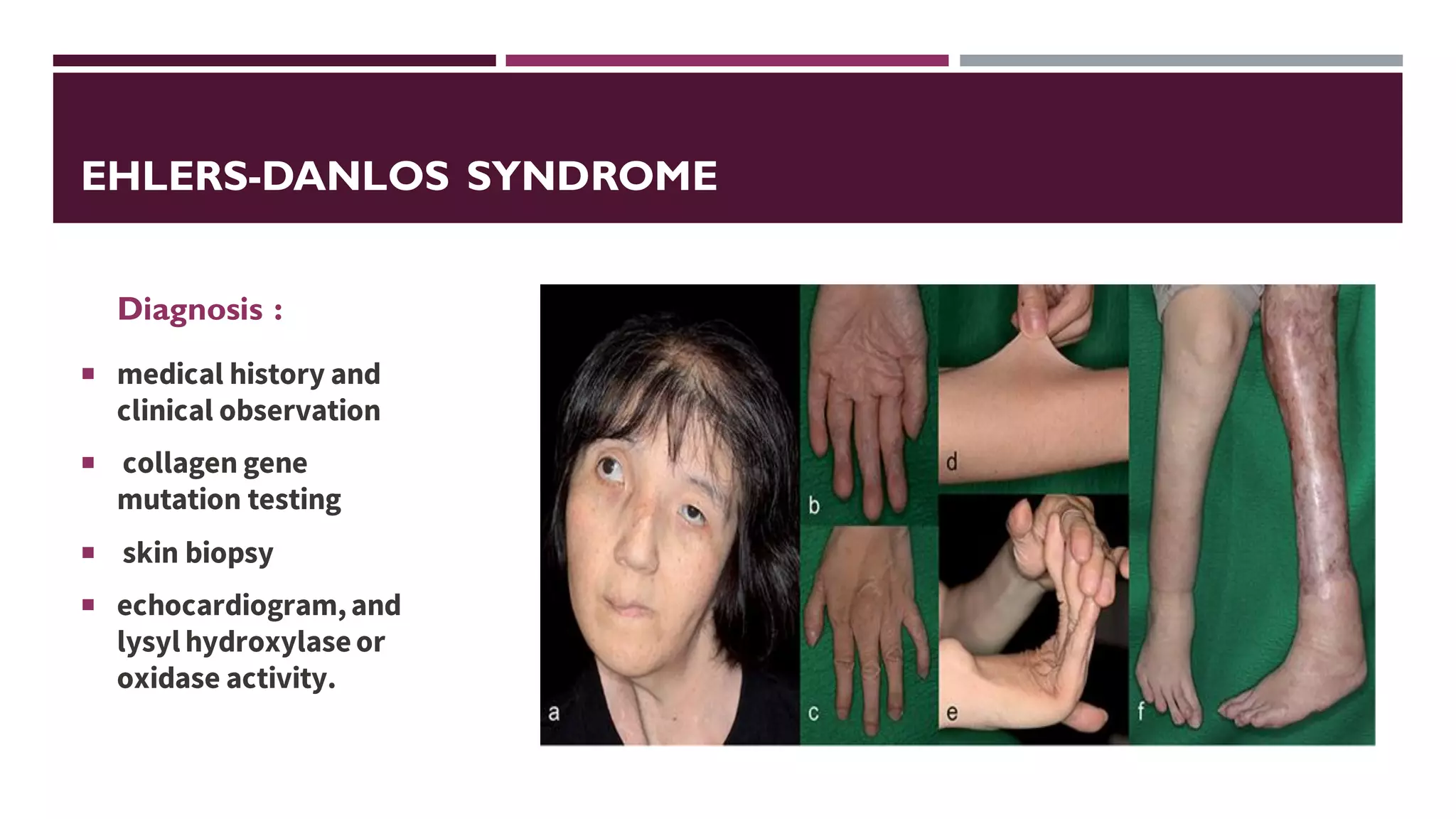
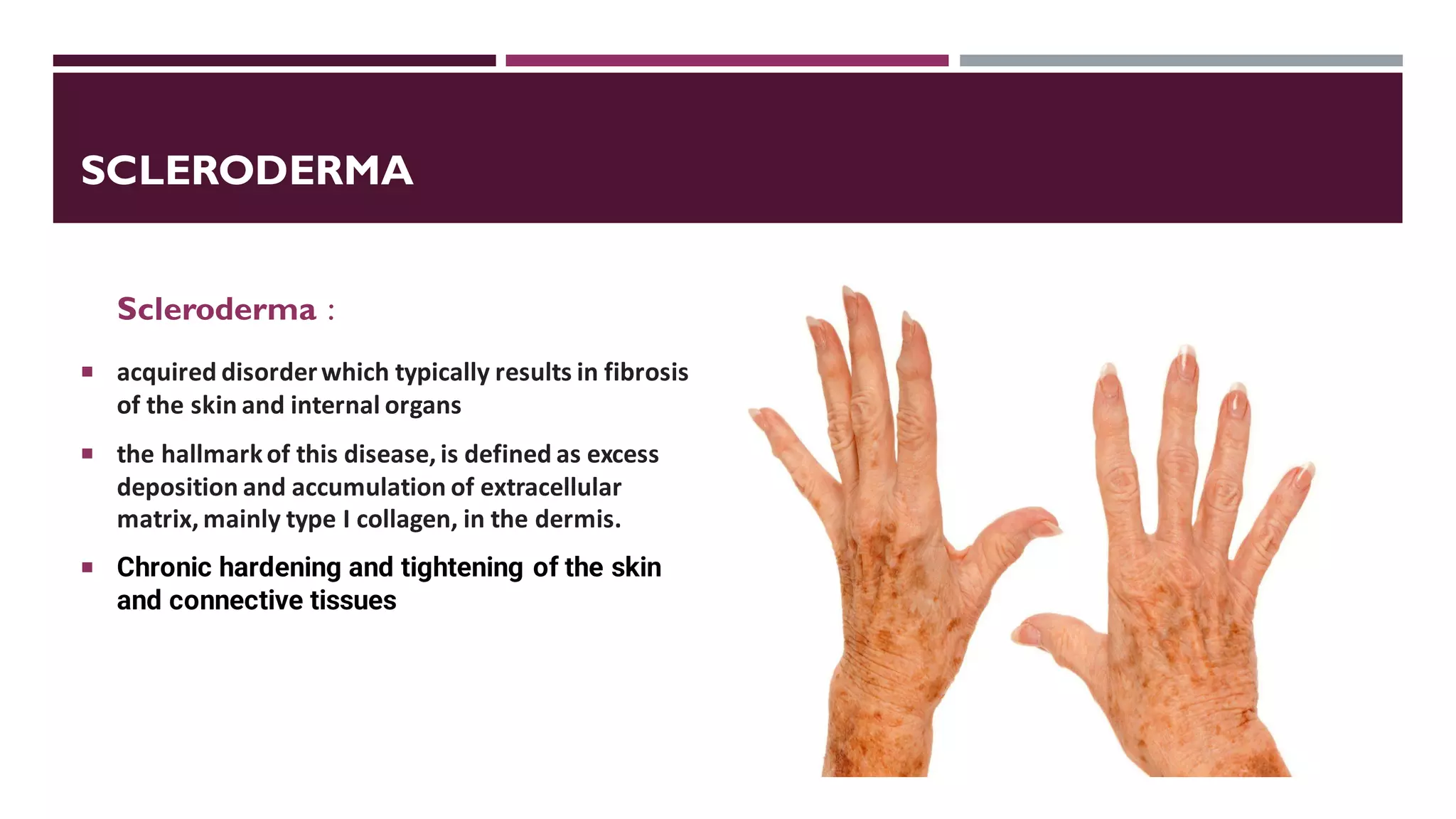
Collagen is the most abundant protein in mammals and plays an important structural role. There are 28 types of collagen that serve different functions. Collagen disorders can be genetic, autoimmune, or due to other causes. They commonly cause symptoms like skin rashes, fatigue, and joint/muscle pain. Major collagen disorders include Ehlers-Danlos syndrome, lupus, scleroderma, Sjogren's syndrome, and epidermolysis bullosa. Diagnosis involves tests and biopsies while treatment focuses on managing symptoms through medications, physical therapy, and lifestyle changes.