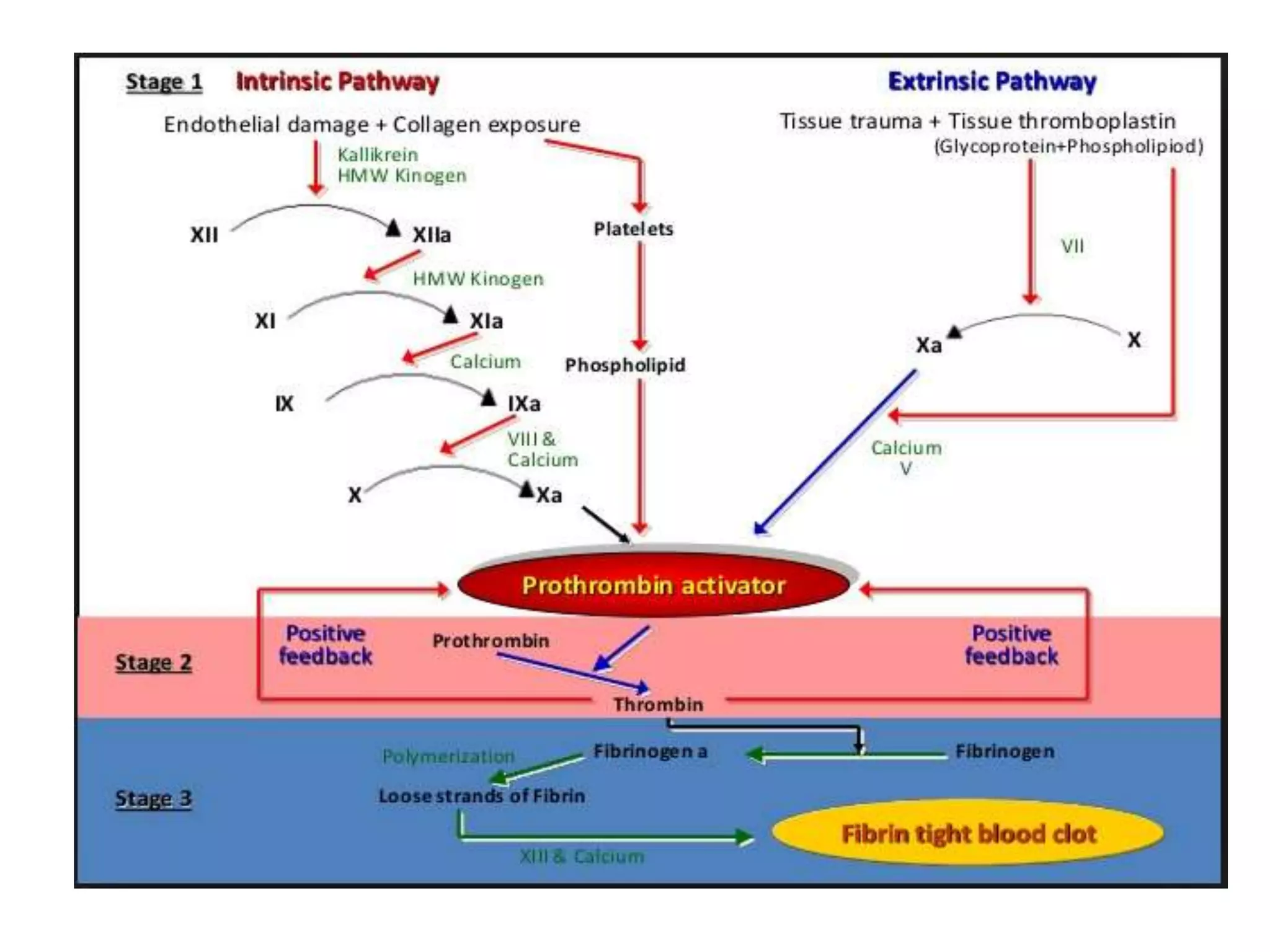
This document discusses coagulation and tests used to evaluate hemostasis and bleeding disorders. It covers the stages of hemostasis, factors involved in coagulation, tests for platelet count, bleeding time, prothrombin time, activated partial thromboplastin time, fibrinogen, and coagulation factor assays. An approach to evaluating a patient with abnormal bleeding is also outlined.