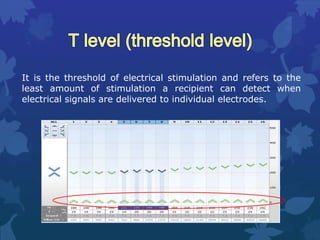
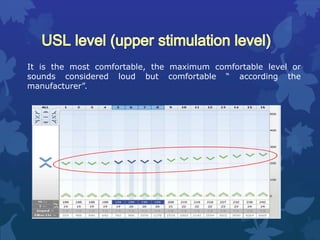
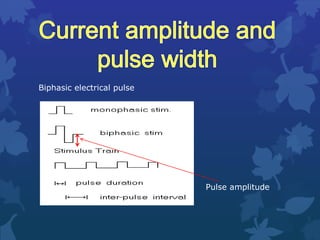
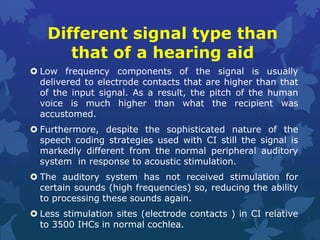
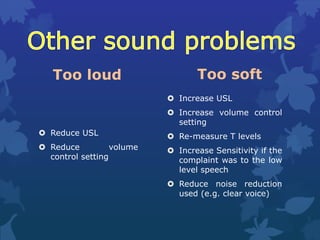
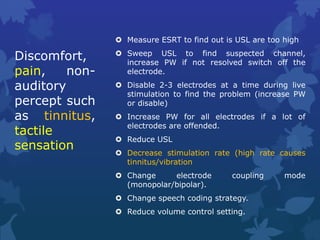
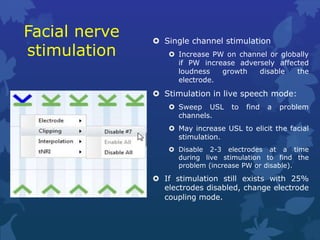
This document discusses various issues that may arise with cochlear implants and potential ways to address patient complaints through programming adjustments. It outlines common complaints such as sound quality issues, discomfort, loudness problems, and facial nerve stimulation. For each complaint, it lists potential programming parameters that could be modified, such as stimulus levels, filter settings, electrode configurations, and coding strategies. It emphasizes considering an acclimatization period and reassessing programming over time before making changes. It also discusses soft failures where performance declines despite normal integrity testing.