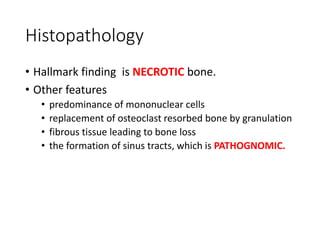
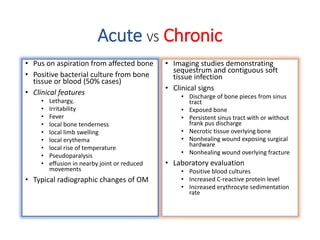
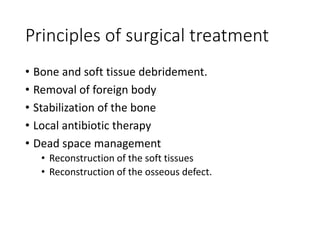
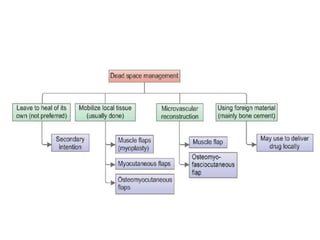
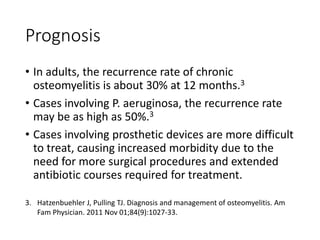
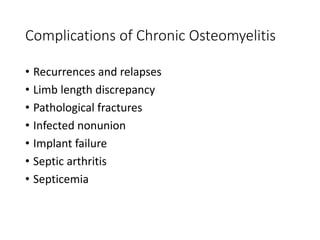
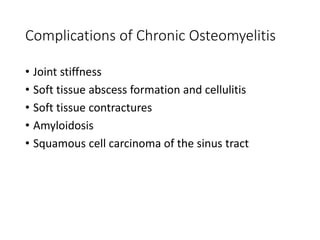
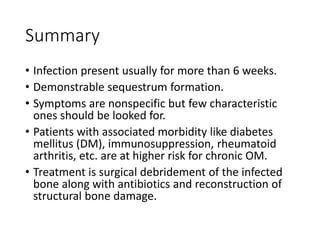
Chronic osteomyelitis is a bone infection that has persisted for over 6 weeks. It is characterized by the formation of necrotic bone fragments called sequestrum. Symptoms are nonspecific but may include pain, swelling, and draining sinuses. Treatment involves surgical debridement of infected bone along with long-term antibiotics to address this difficult to treat infection that has high recurrence rates and causes significant bone and tissue damage over time.