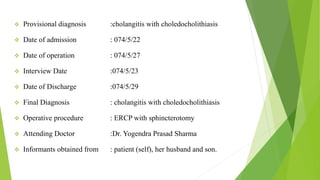
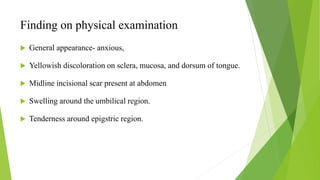
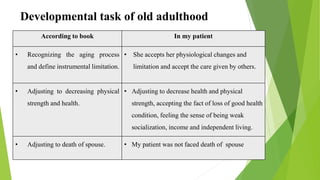
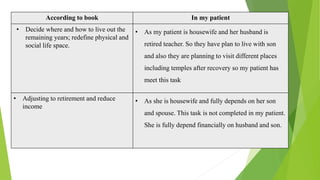
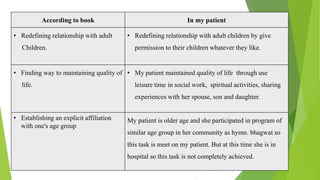
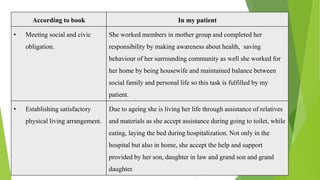
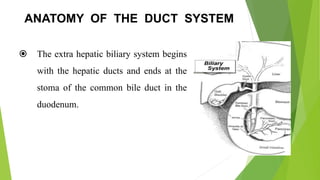
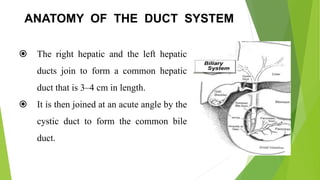
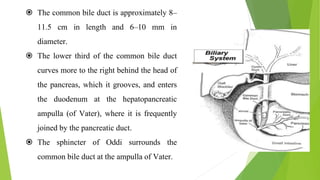
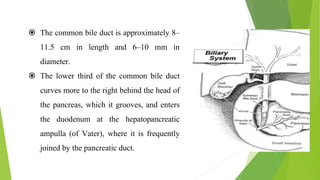
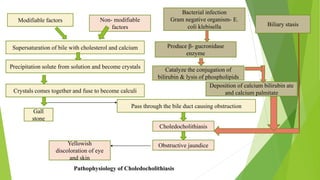
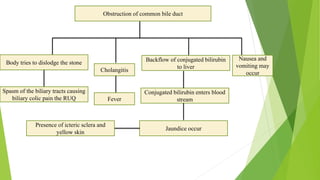
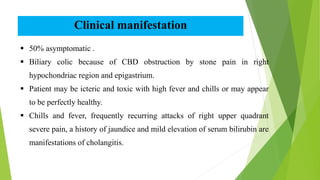
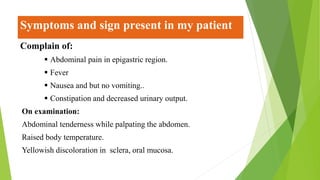
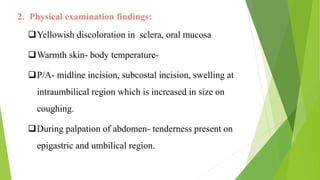
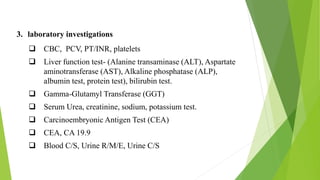
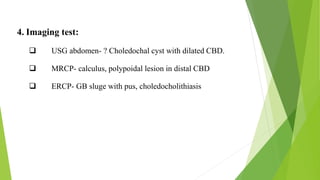
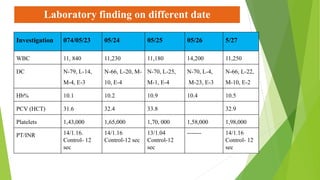
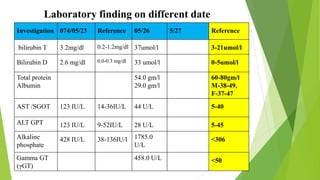
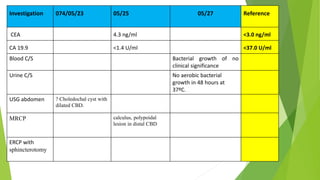
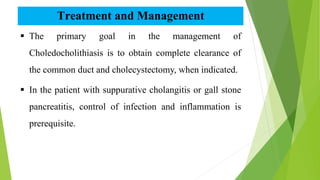
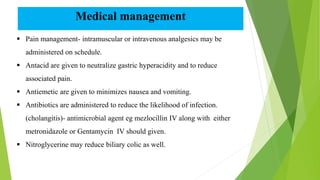
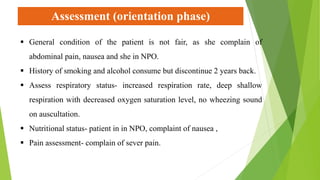
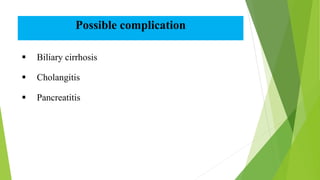
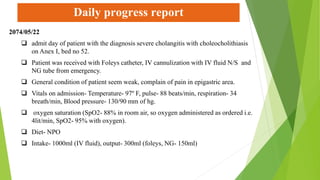
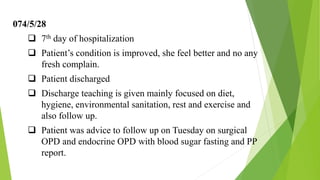
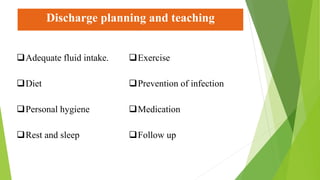
The case study investigates a patient with cholangitis and choledocholithiasis, aiming to explore its causes, symptoms, and management while providing holistic nursing care. It includes detailed patient history, clinical manifestations, disease anatomy, and interventions taken, emphasizing collaboration with the healthcare team and family members. Key factors identified are the age-related prevalence of choledocholithiasis and the complexities of managing this condition in an older patient.