This document discusses childhood asthma, including its definition, risk factors, diagnosis, and treatment. Key points include:
- Asthma is a chronic inflammatory airway disorder characterized by variable airflow obstruction and airway hyperresponsiveness.
- Risk factors include genetic predisposition, obesity, allergens, infections, and tobacco smoke.
- Diagnosis is based on symptoms like recurrent wheezing and cough, as well as response to bronchodilators. Spirometry can help diagnose in children over 5.
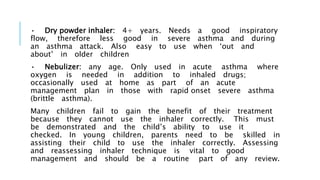
- Treatment involves bronchodilators, inhaled corticosteroids, and other controllers. Correct inhaler technique is important for effective treatment.