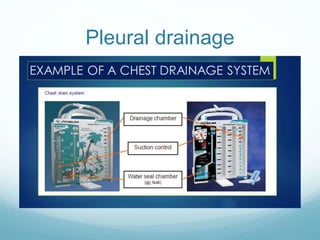
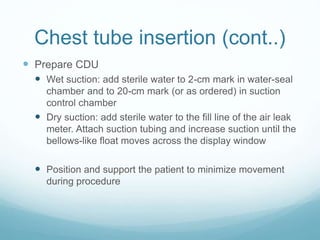
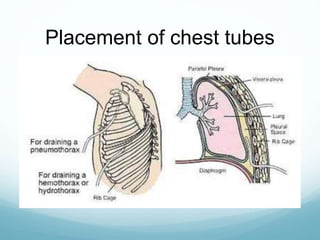
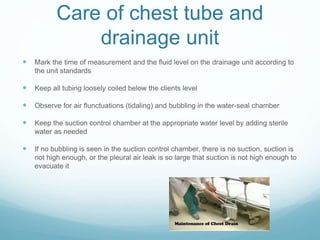
Chest tubes are hollow, flexible tubes placed in the chest to drain fluid, air, or blood from the pleural space between the lungs and chest wall. They connect to a chest drainage unit which uses suction and a water seal system to drain the pleural space. Chest tubes are used to treat conditions like pneumothorax, hemothorax, and pleural effusions. They are inserted through the ribs into the pleural space and connected to a drainage unit. Nurses monitor tube function and drainage amount and ensure the drainage system remains intact until the tube can be removed by a physician once drainage decreases.