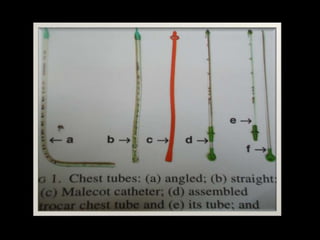
This document discusses intercostal drainage, including indications for chest drain insertion such as pneumothorax, malignant pleural effusion, and empyema. It describes different techniques for chest drain insertion including guidewire, trocar, and open/operating methods. Factors such as drain size, positioning, and drainage systems including one bottle, two bottle, and suction systems are covered. Complications and recommendations for safe practice are also summarized.