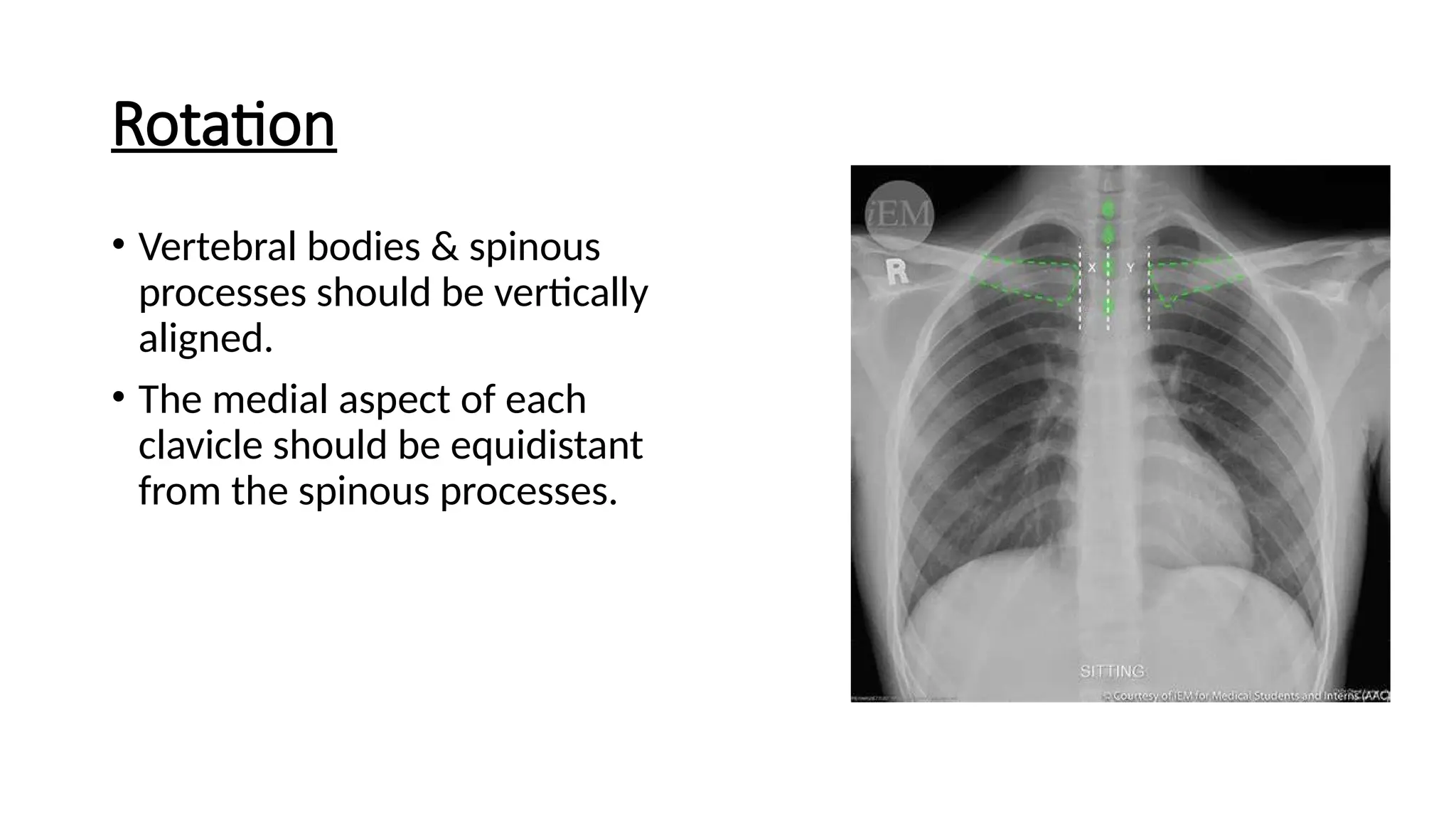
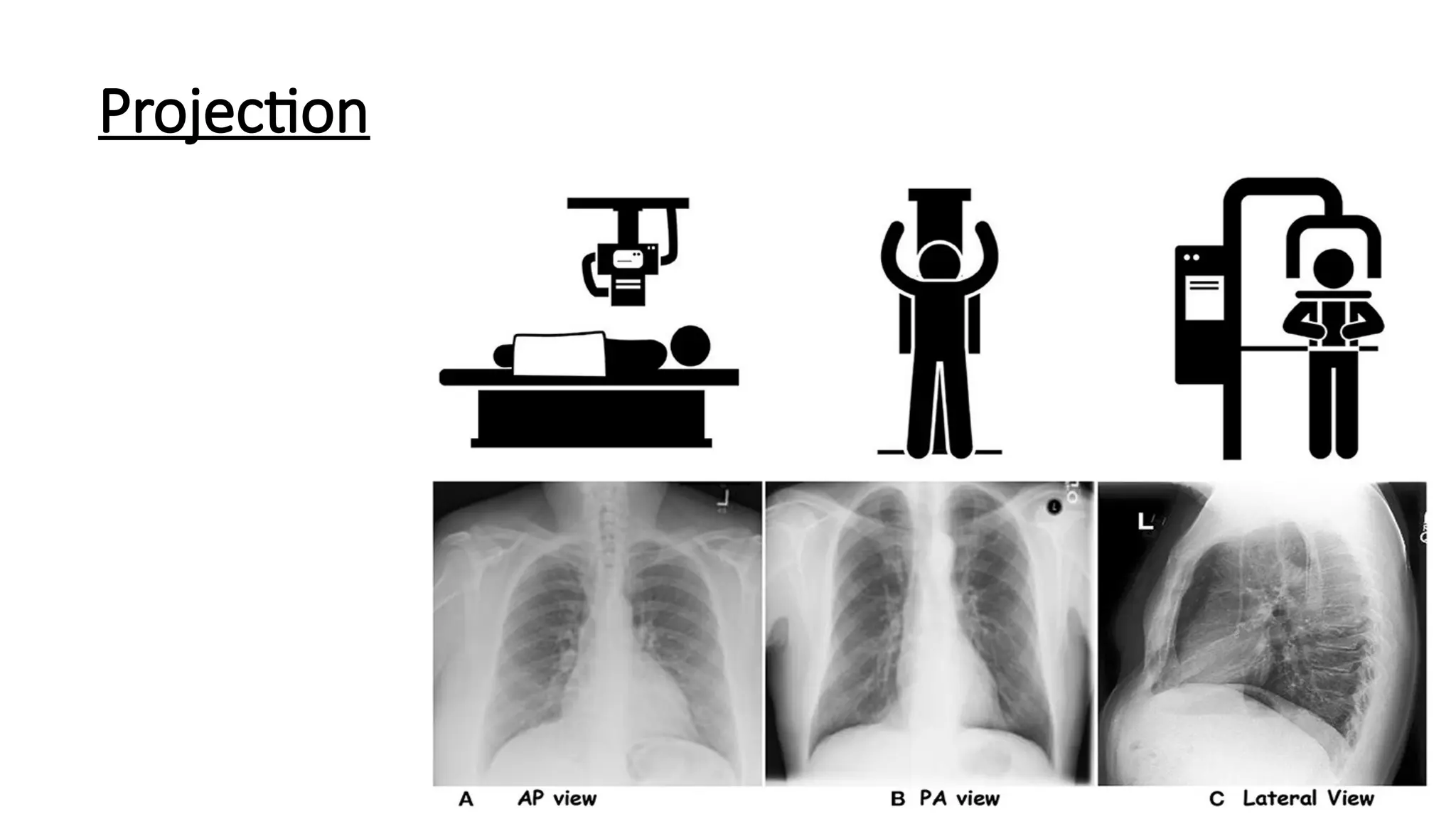
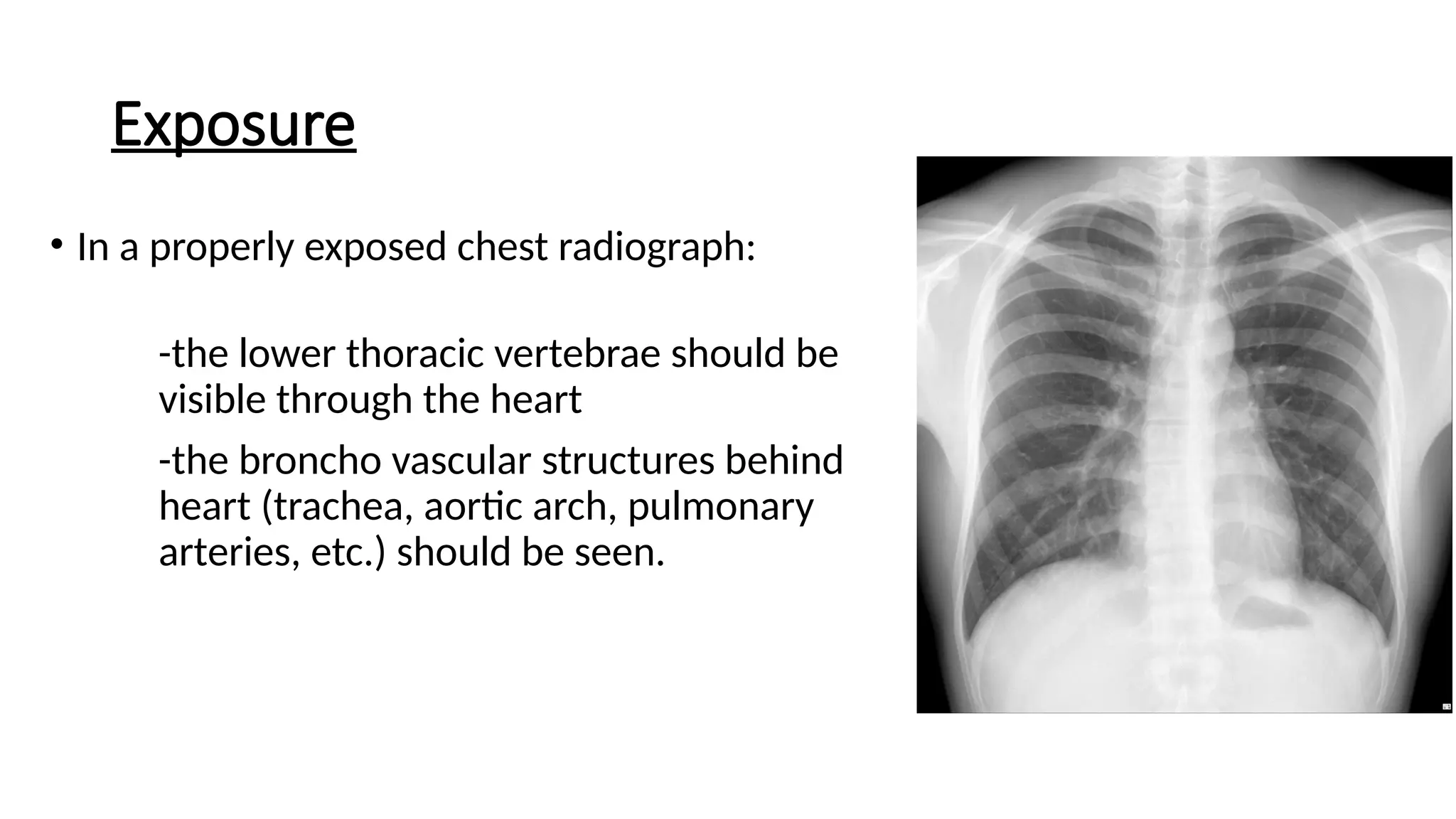
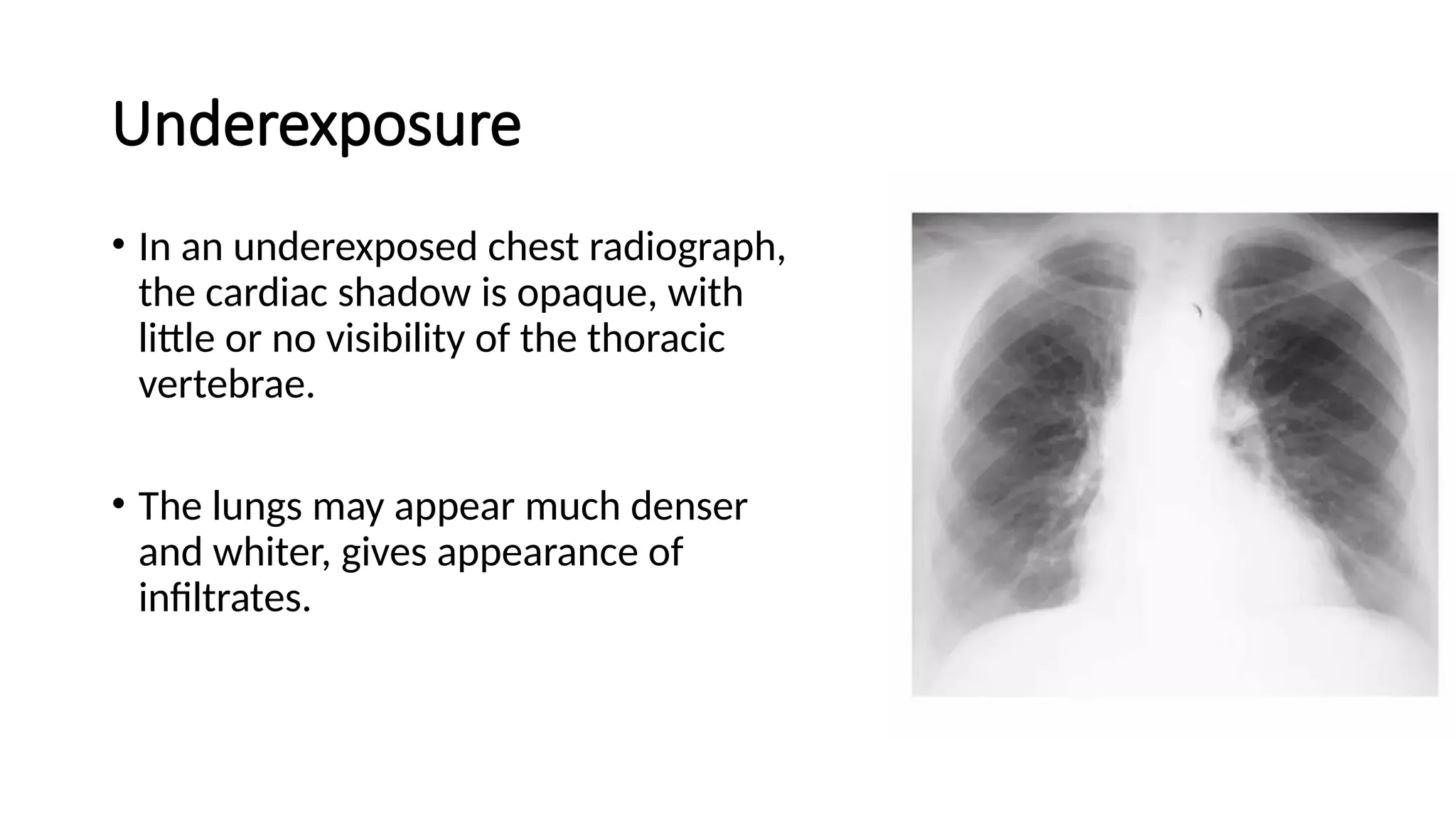
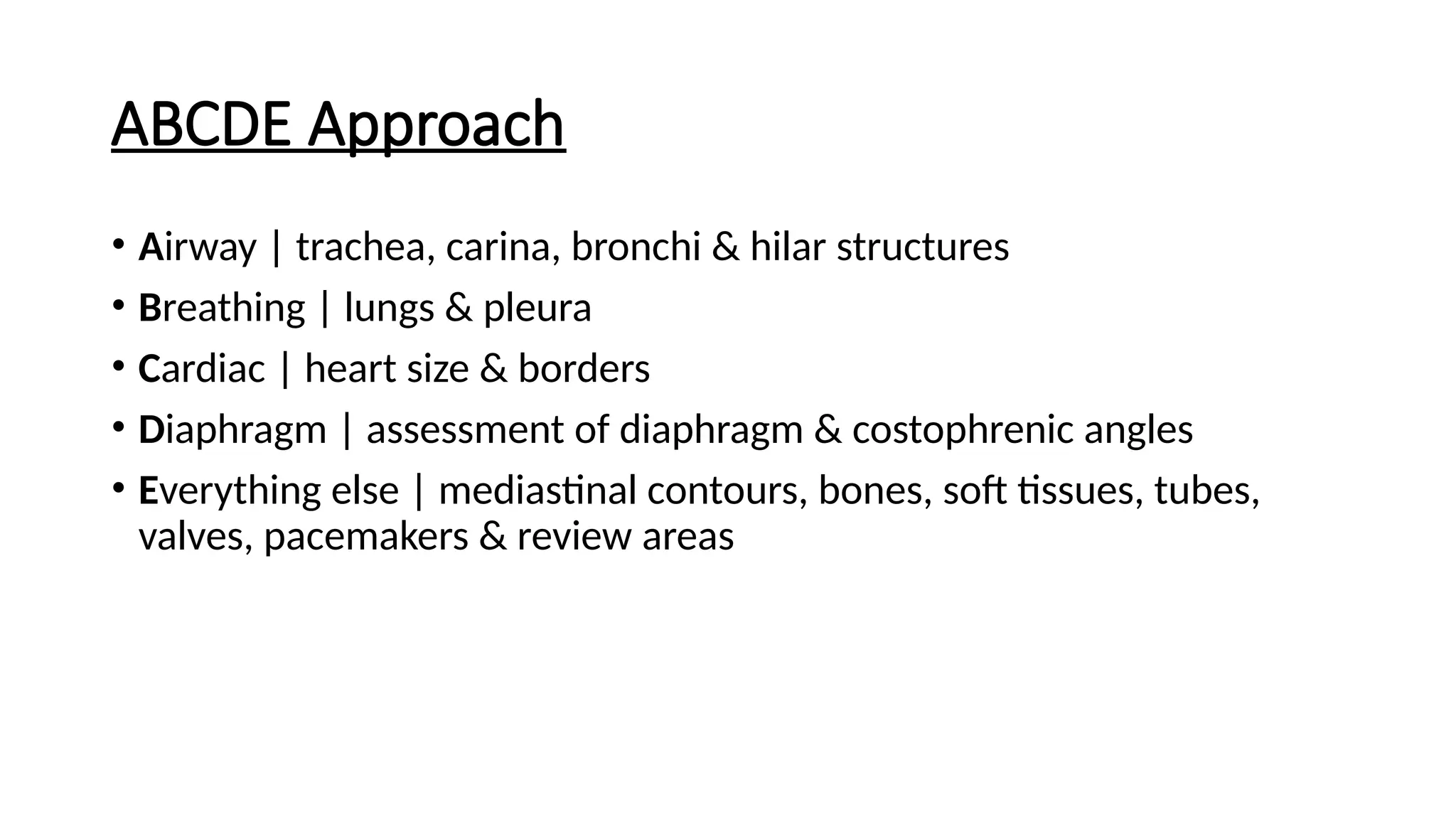
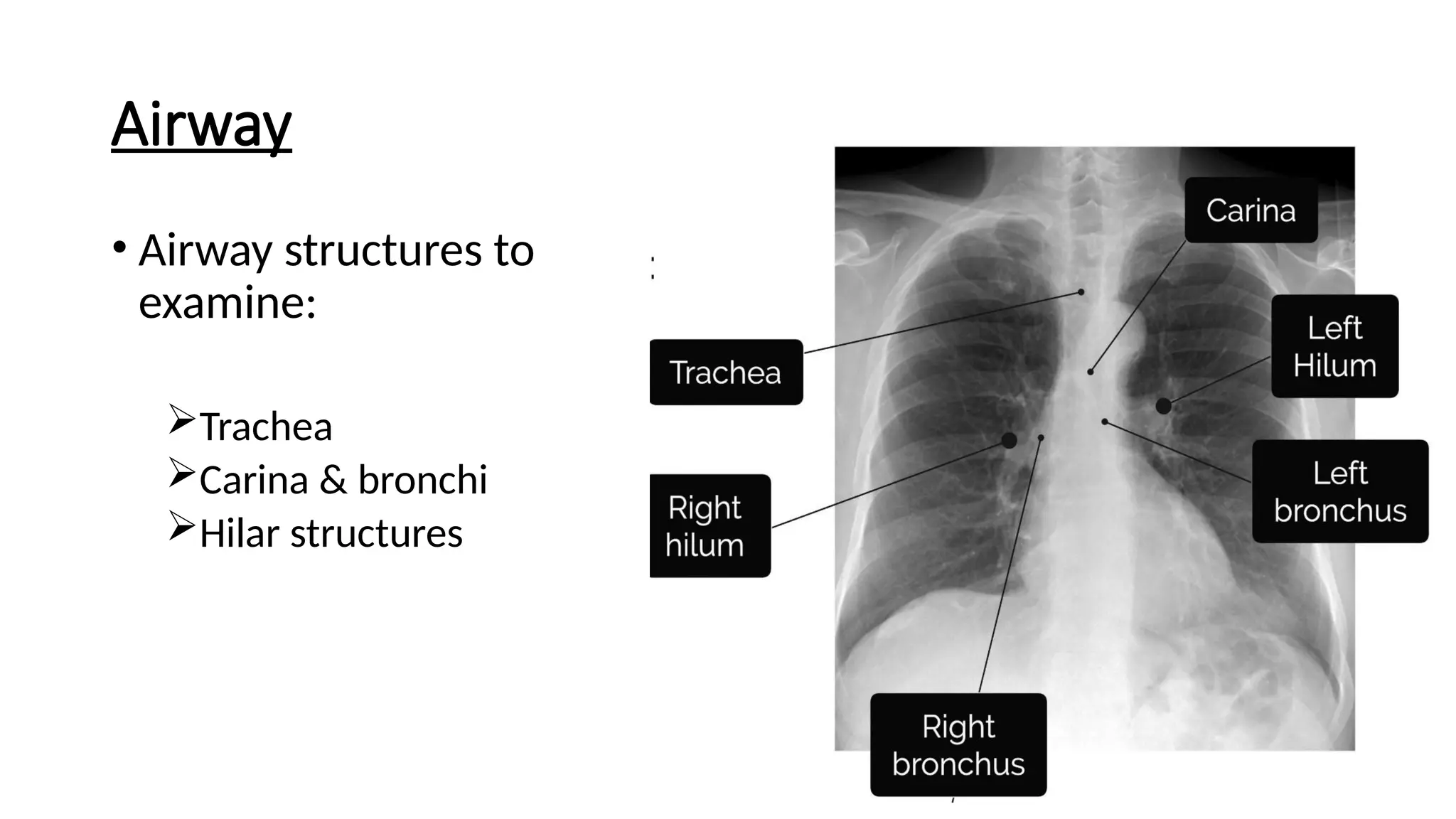
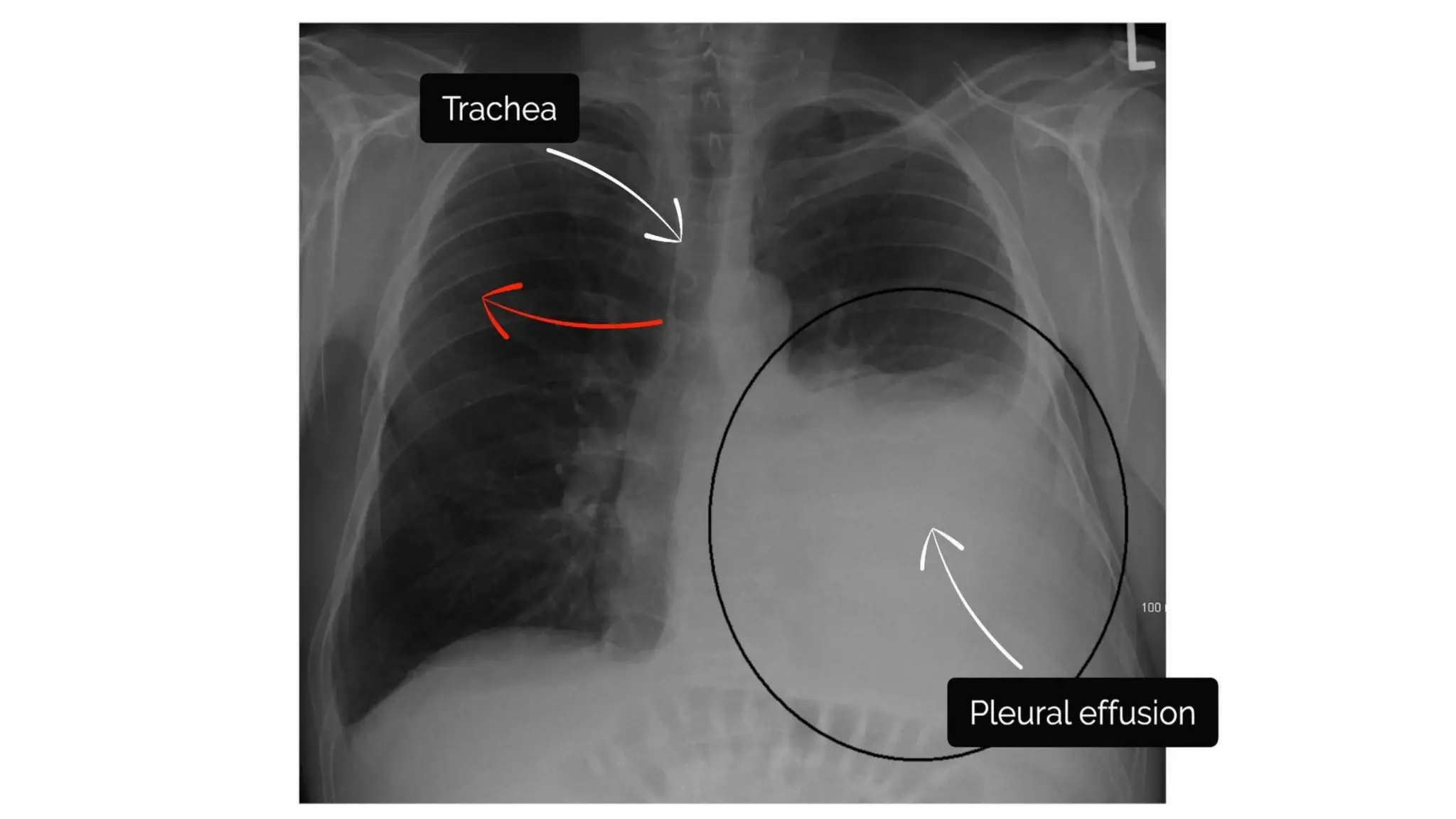
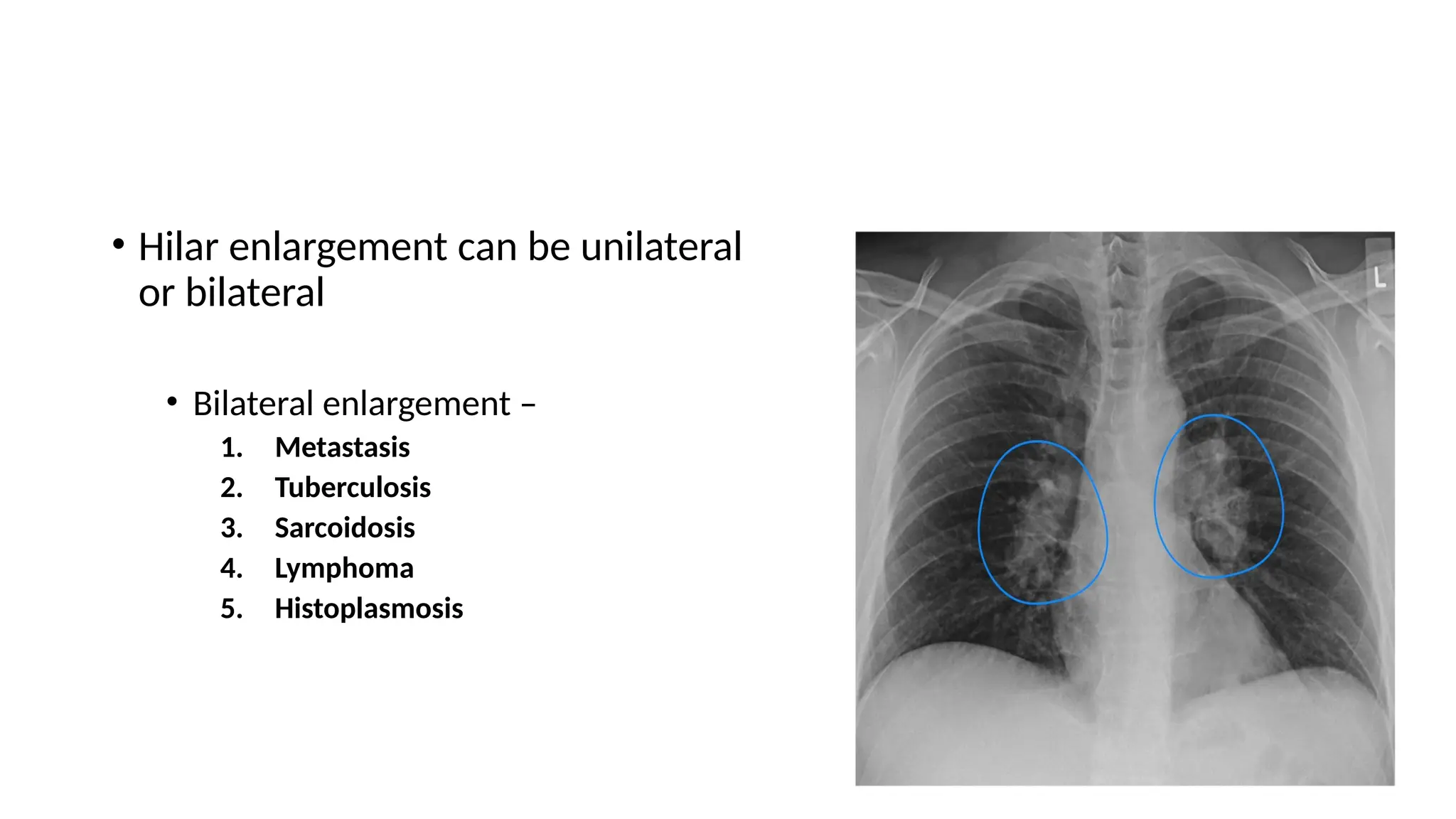
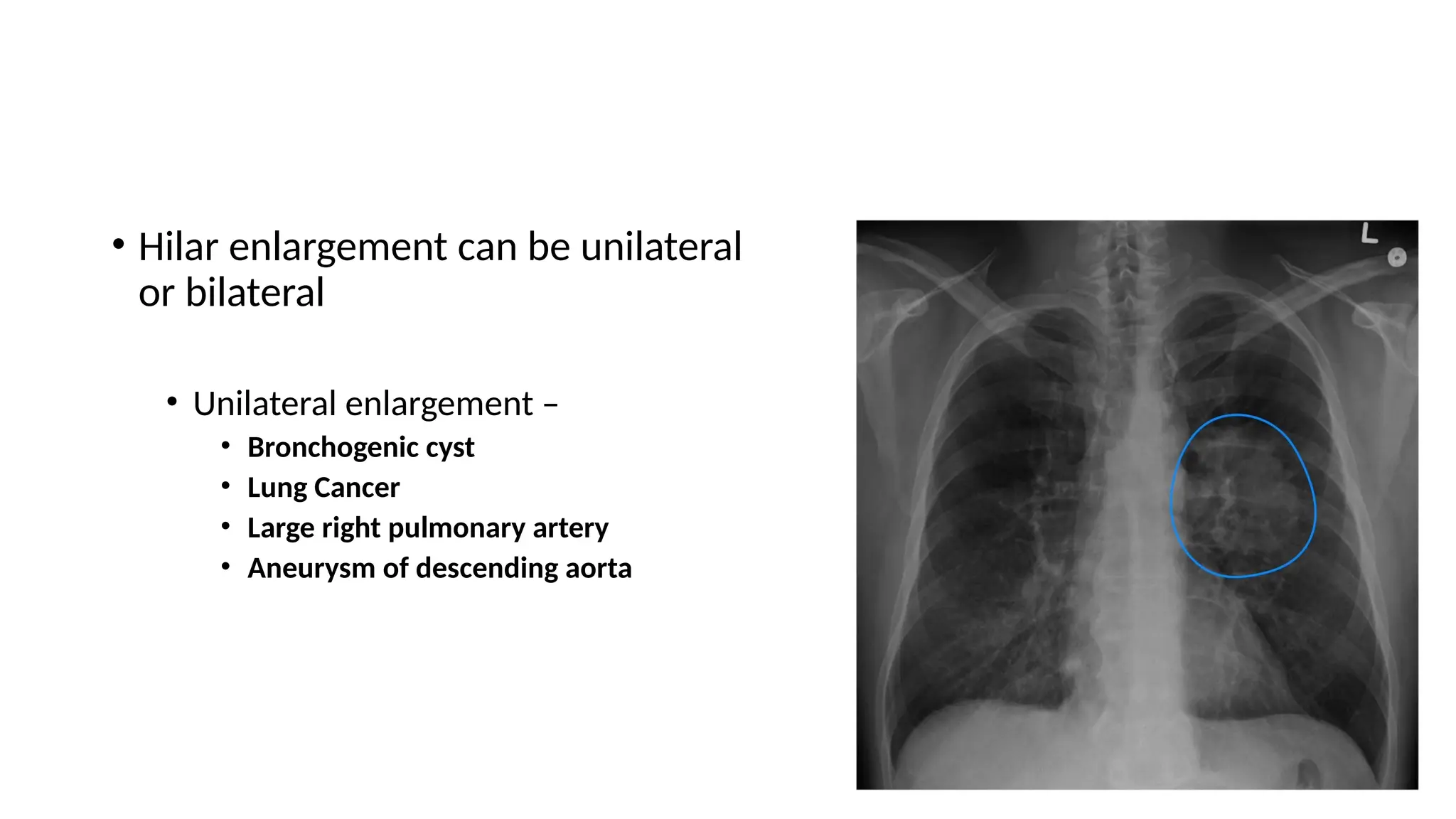
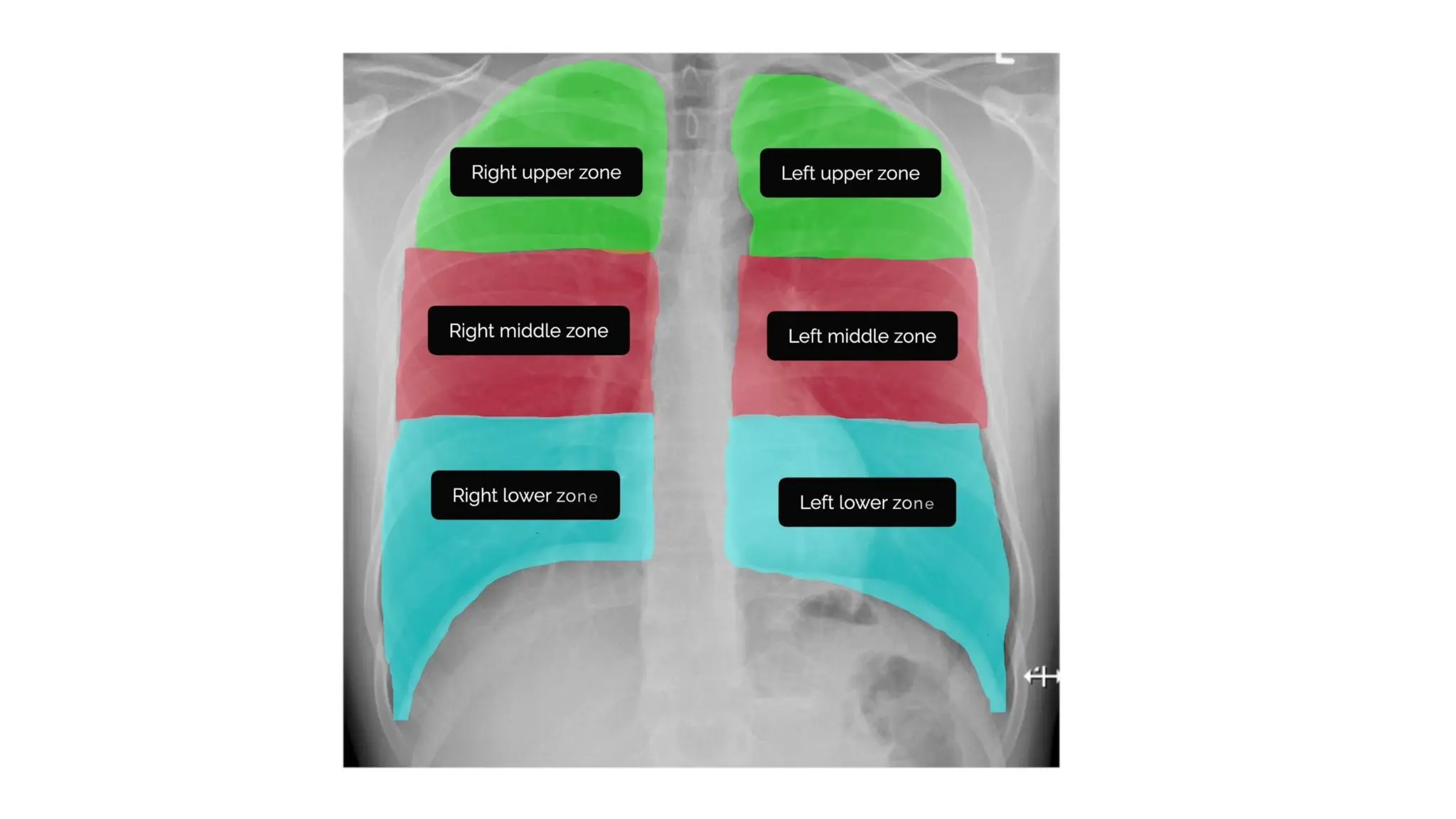
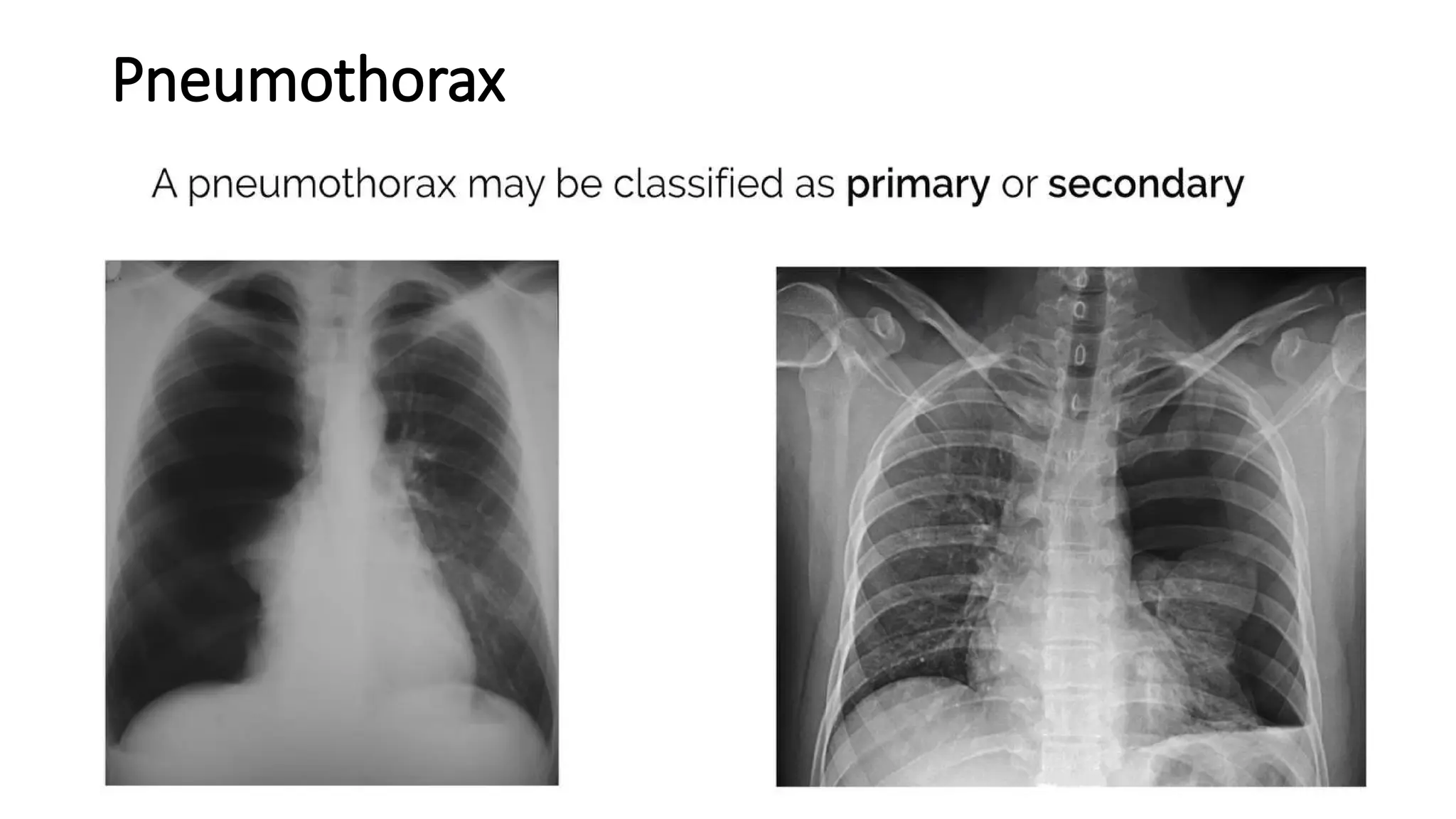
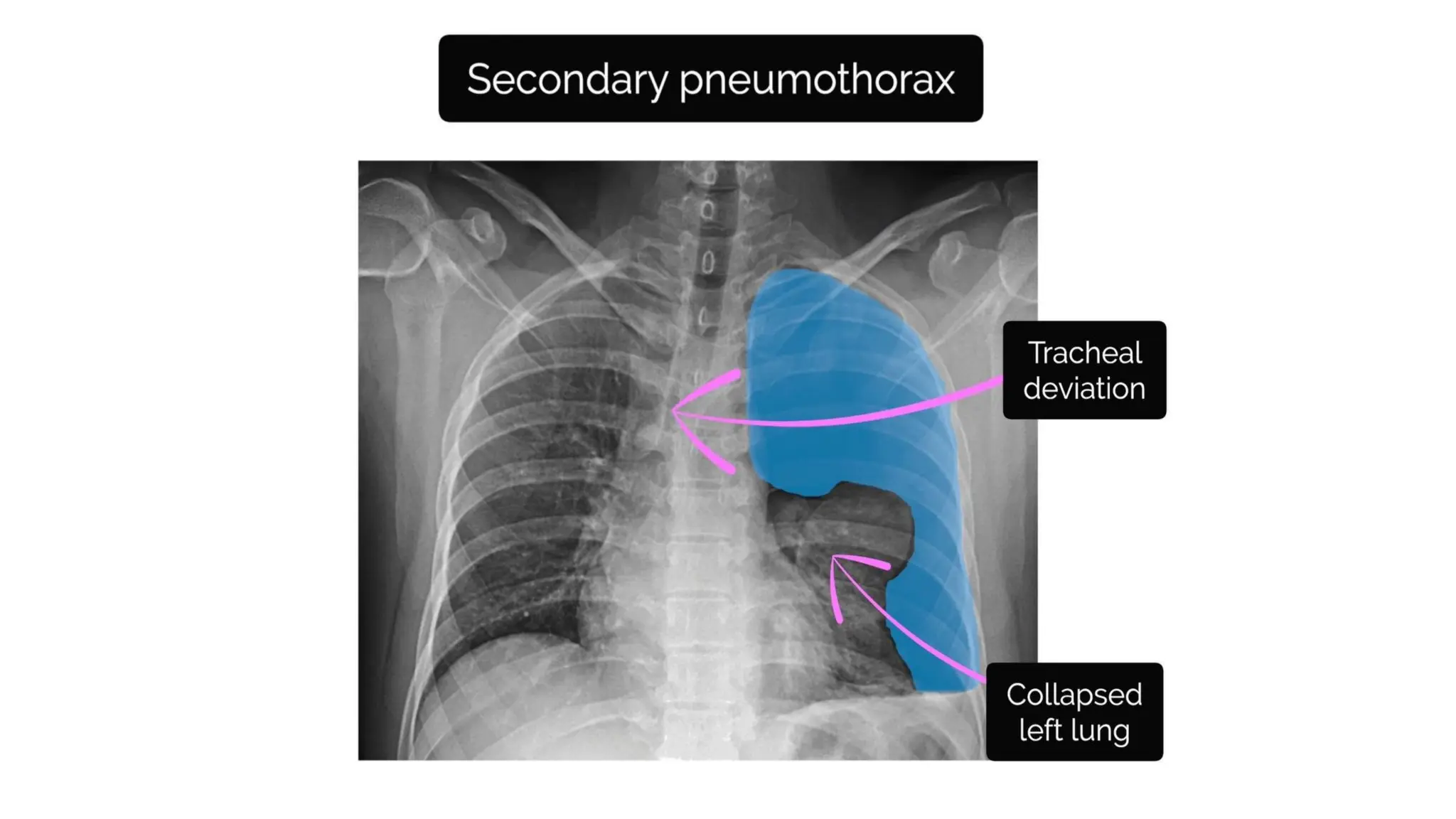
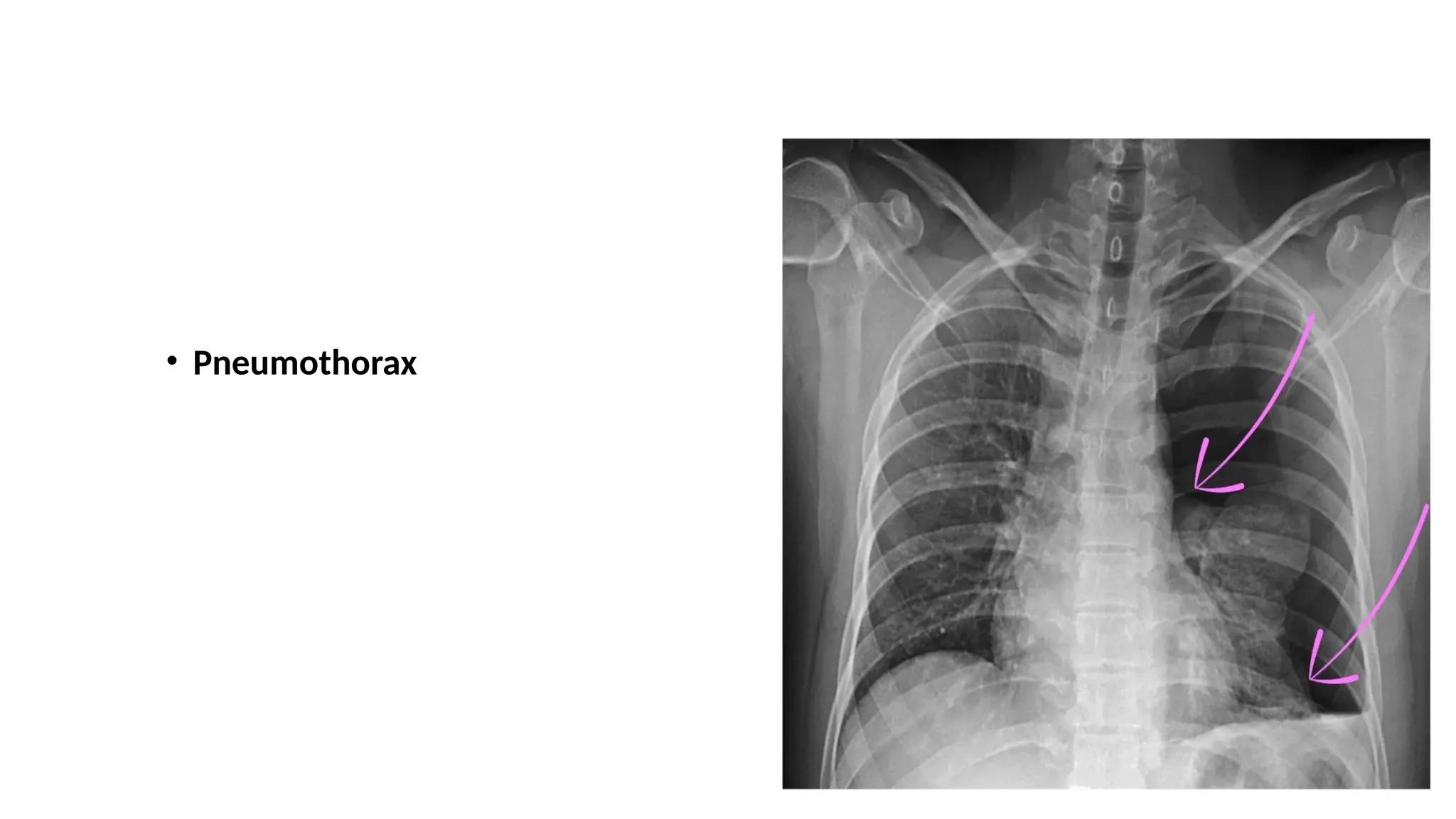
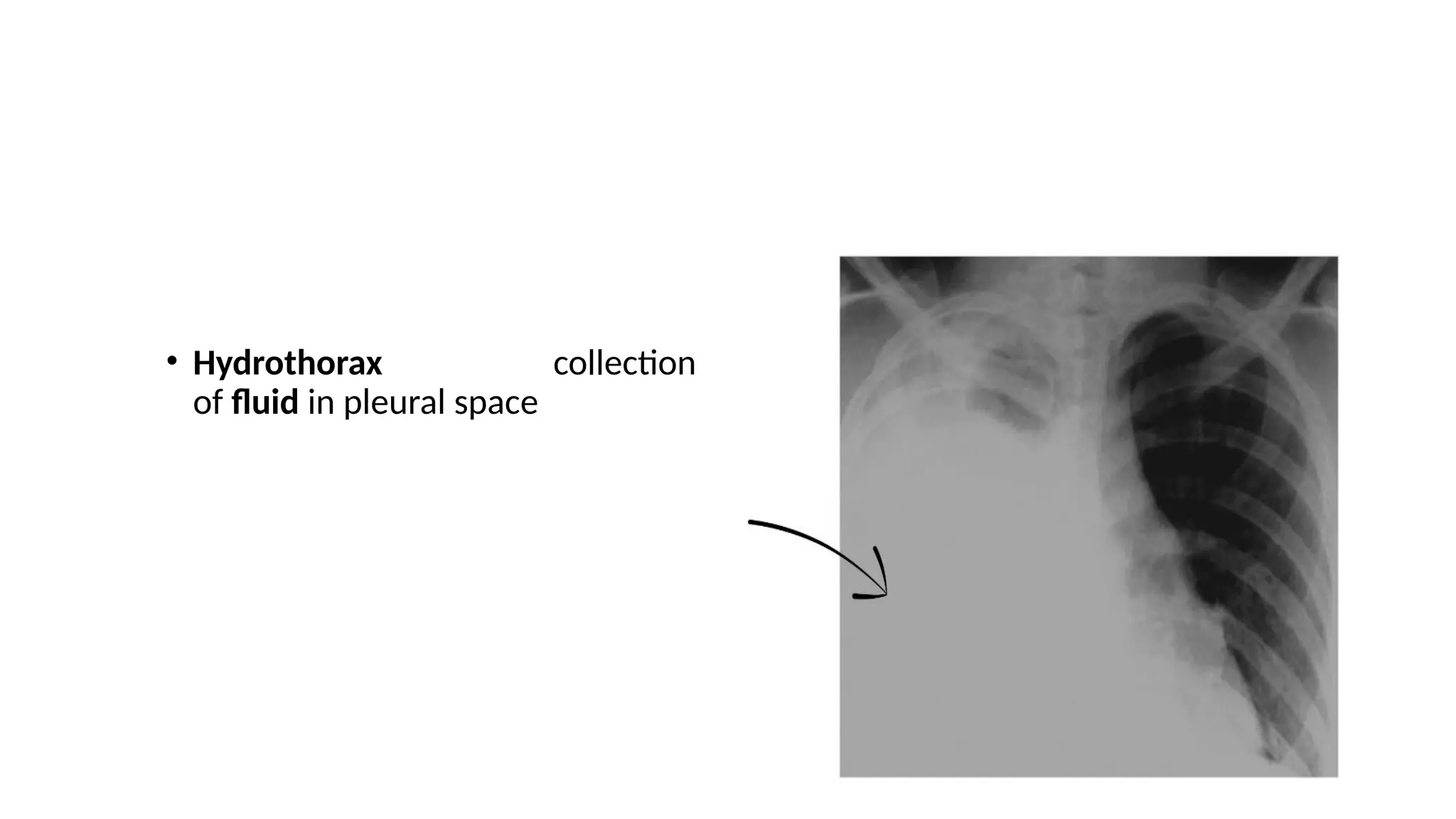
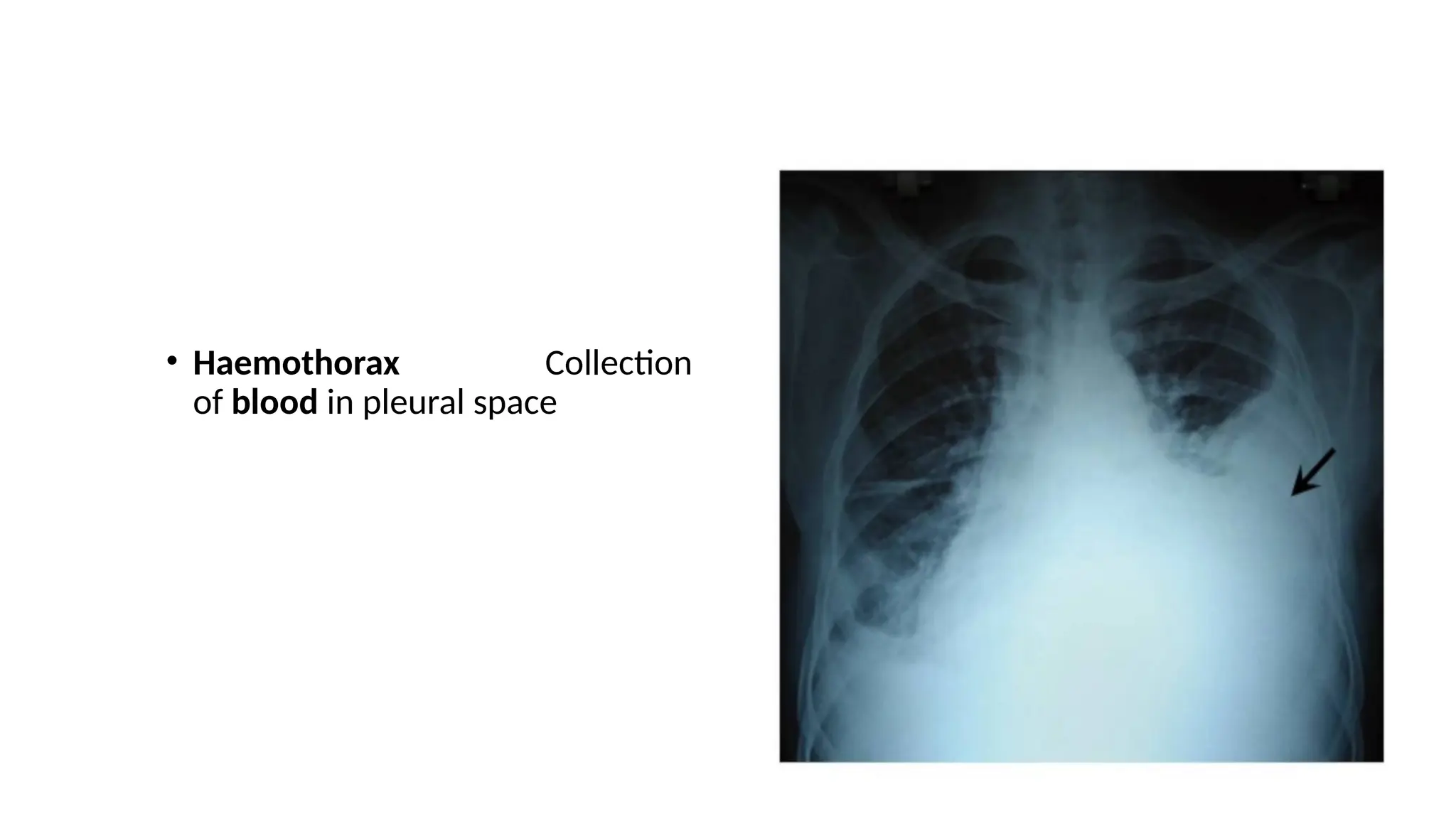
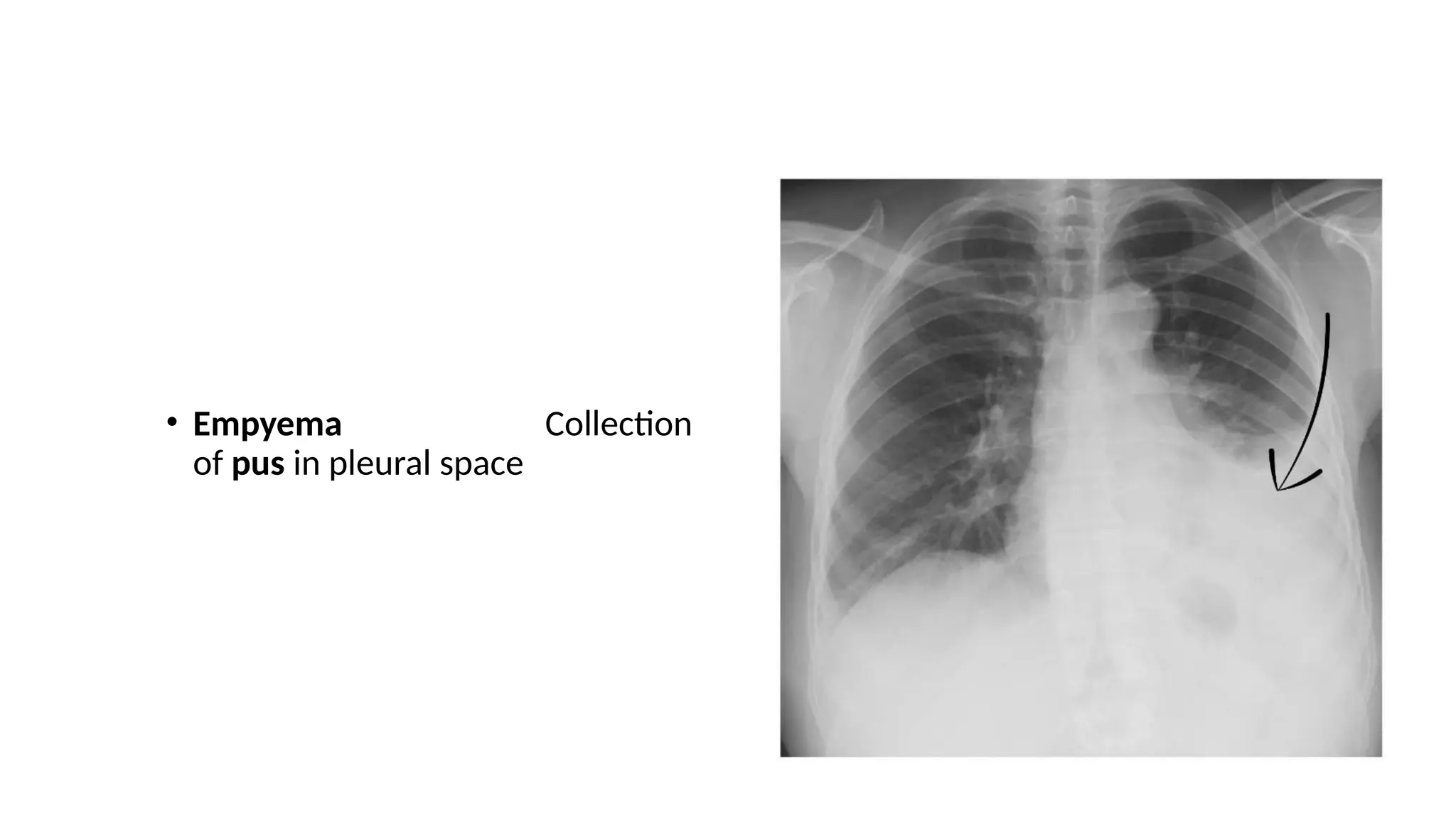
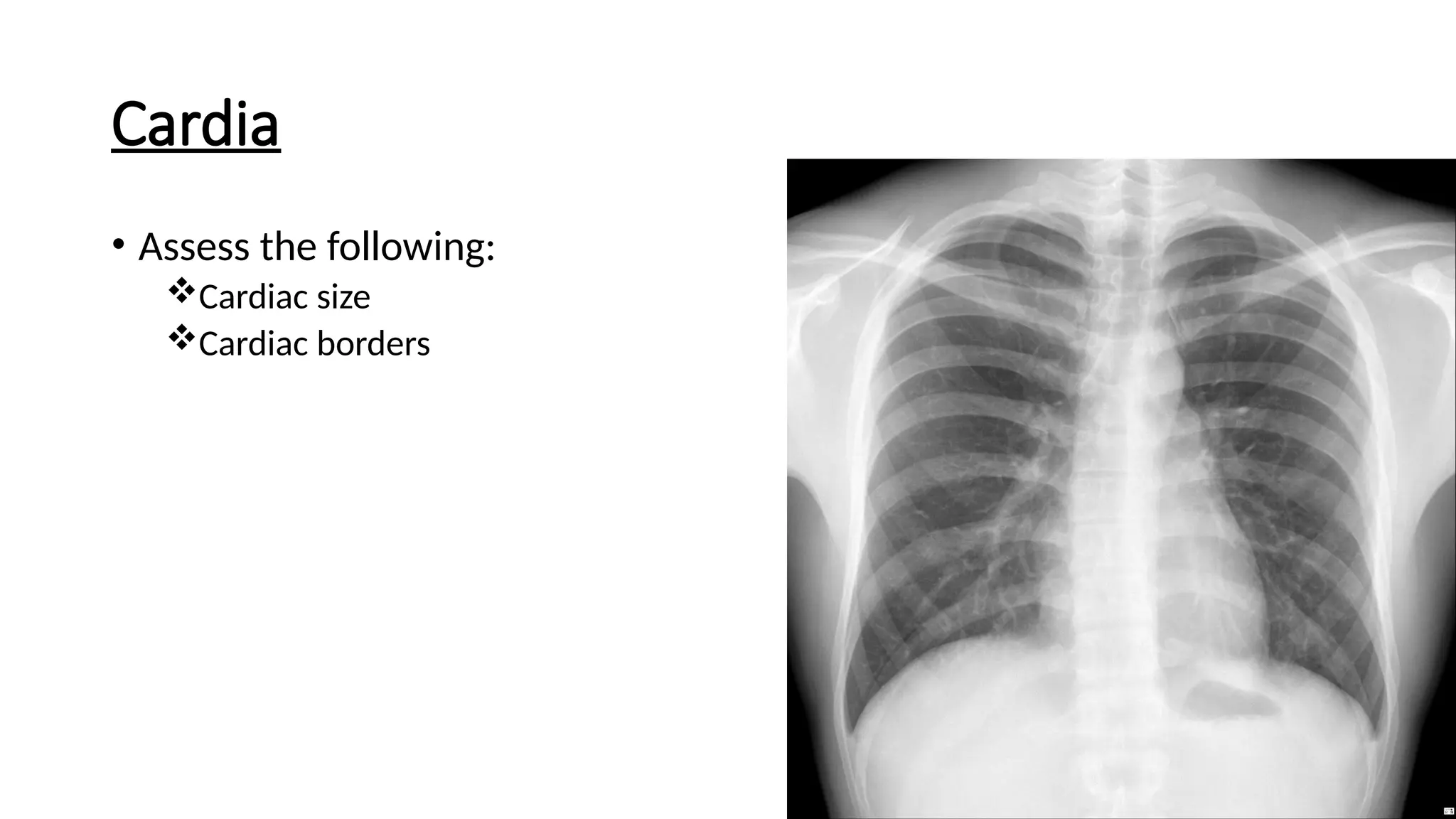
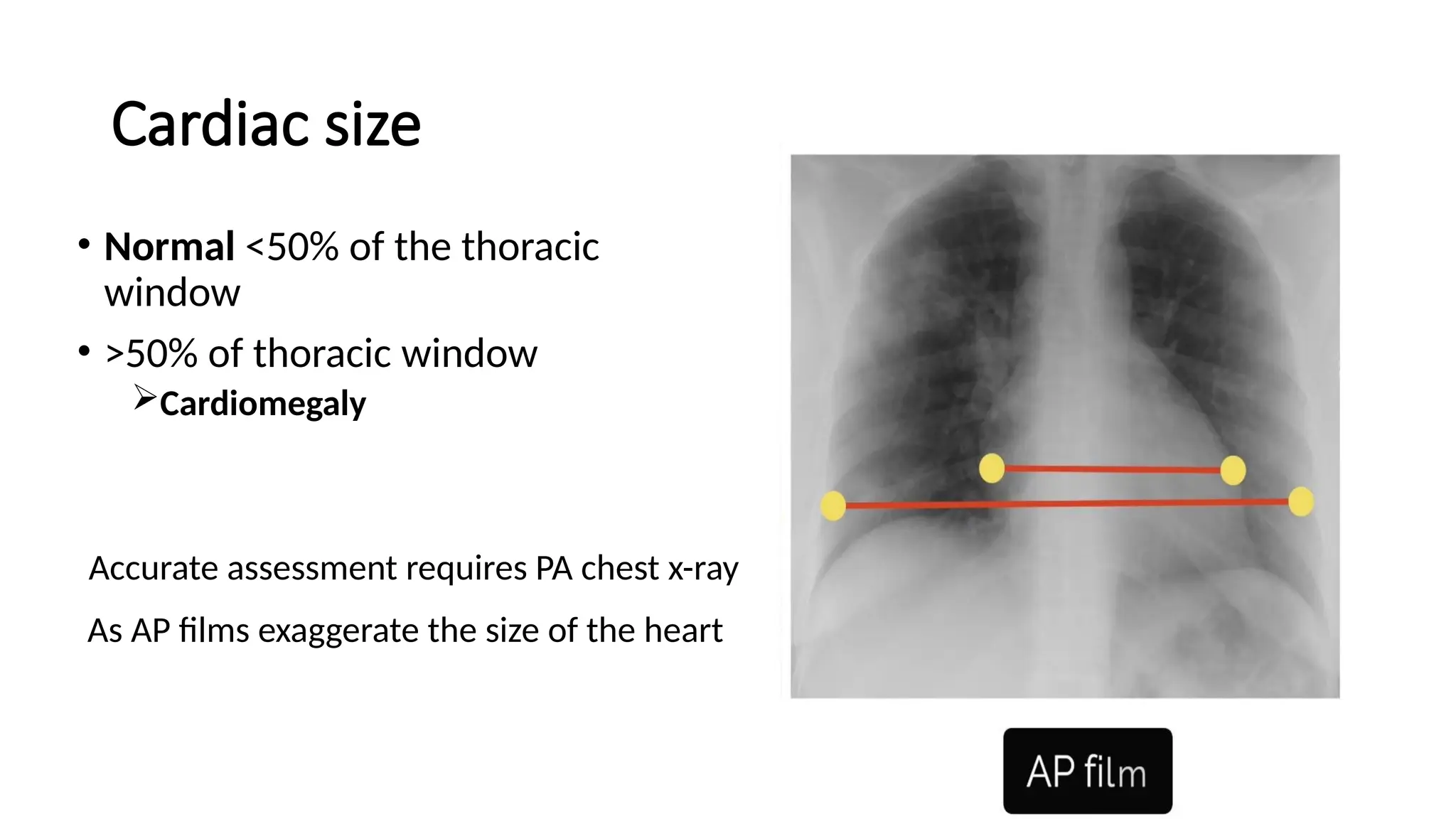
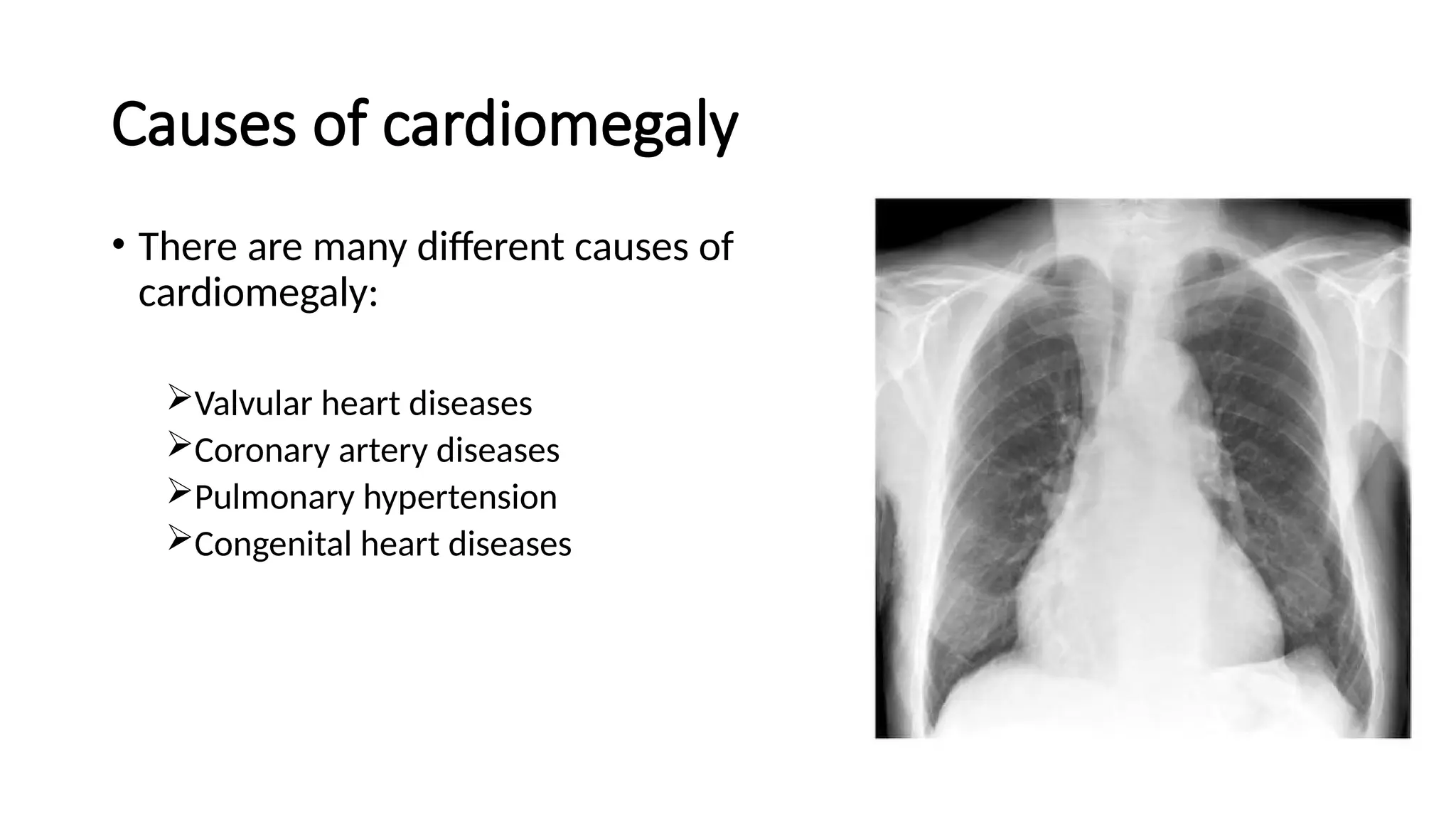
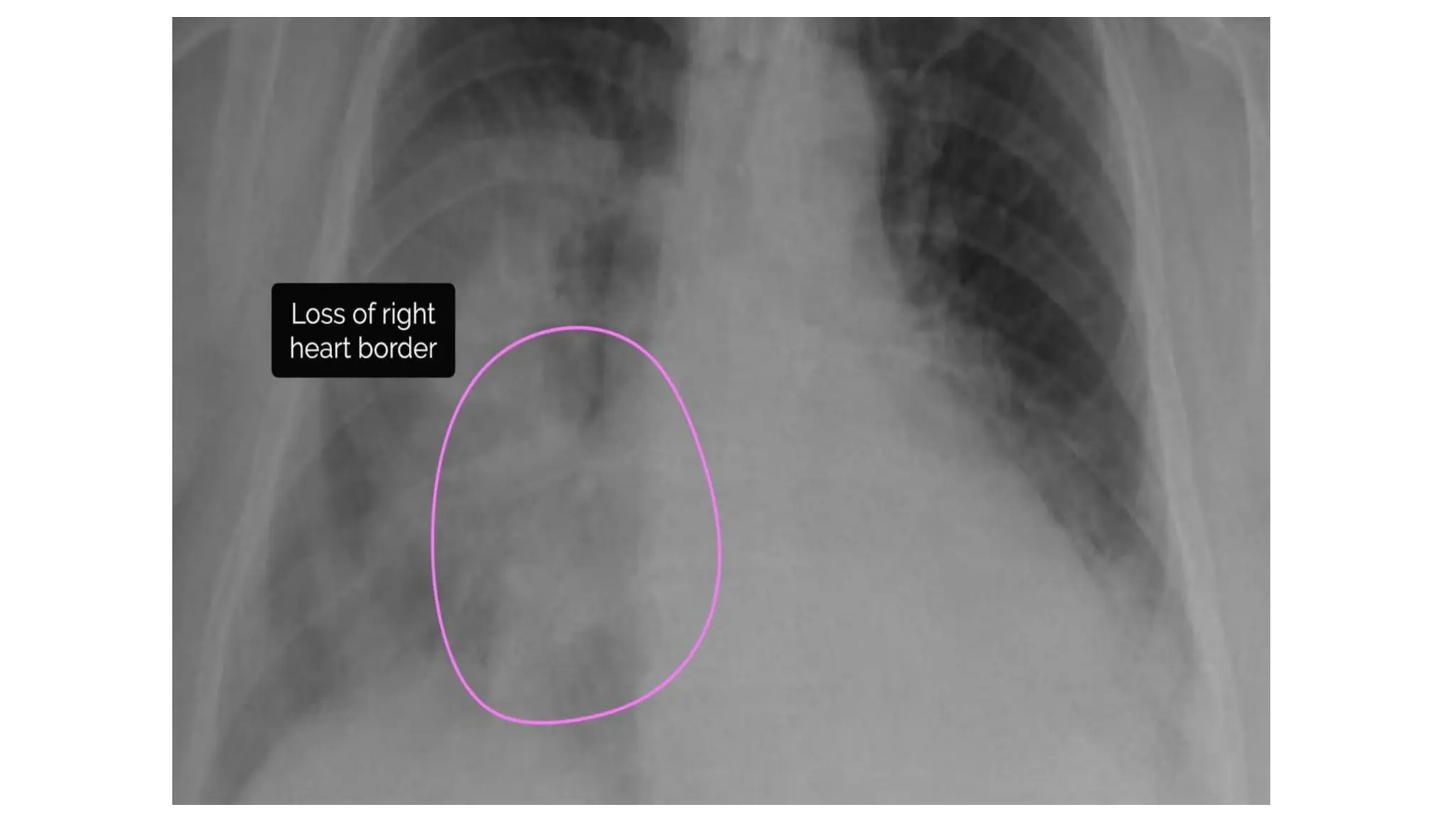
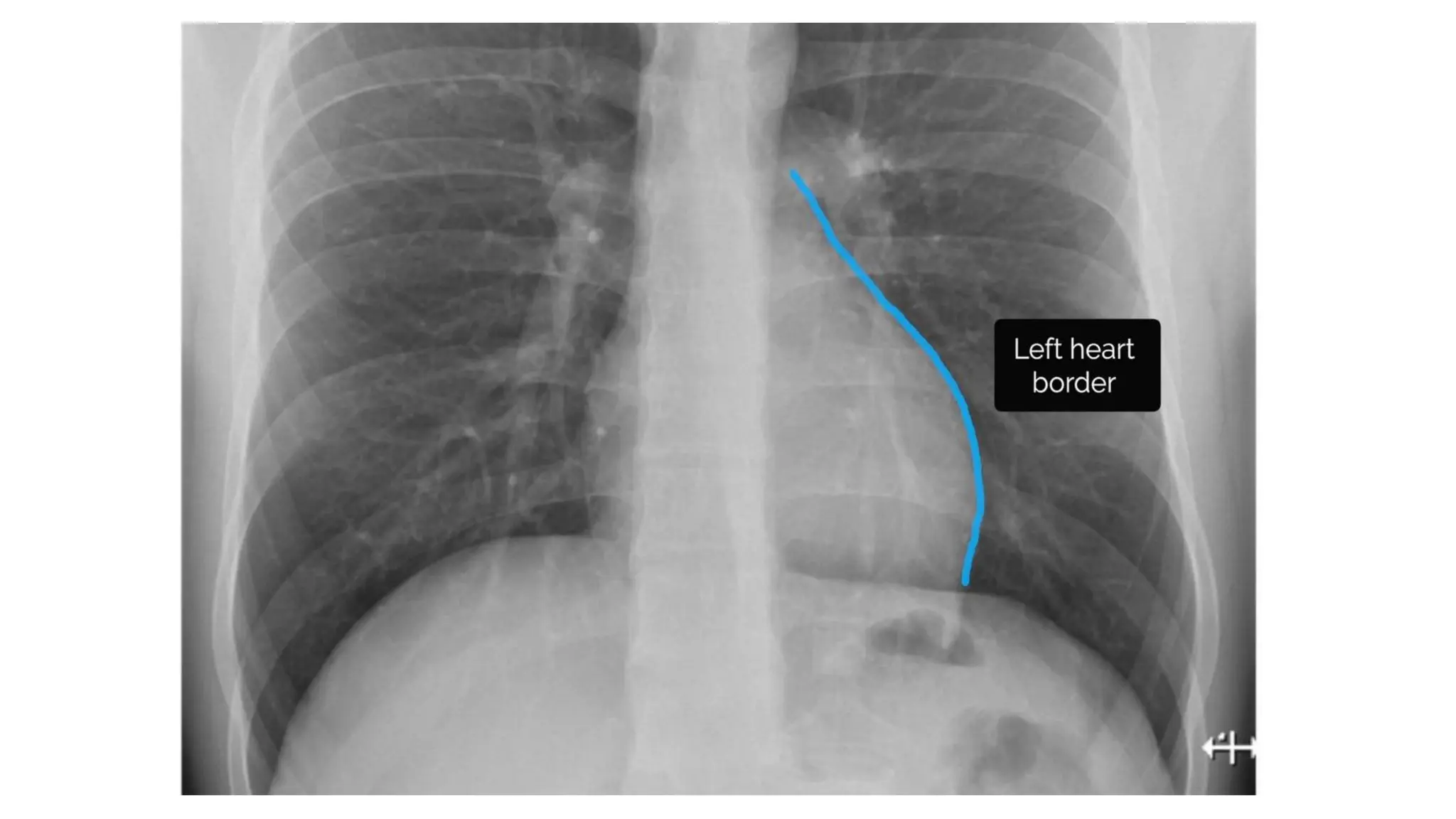
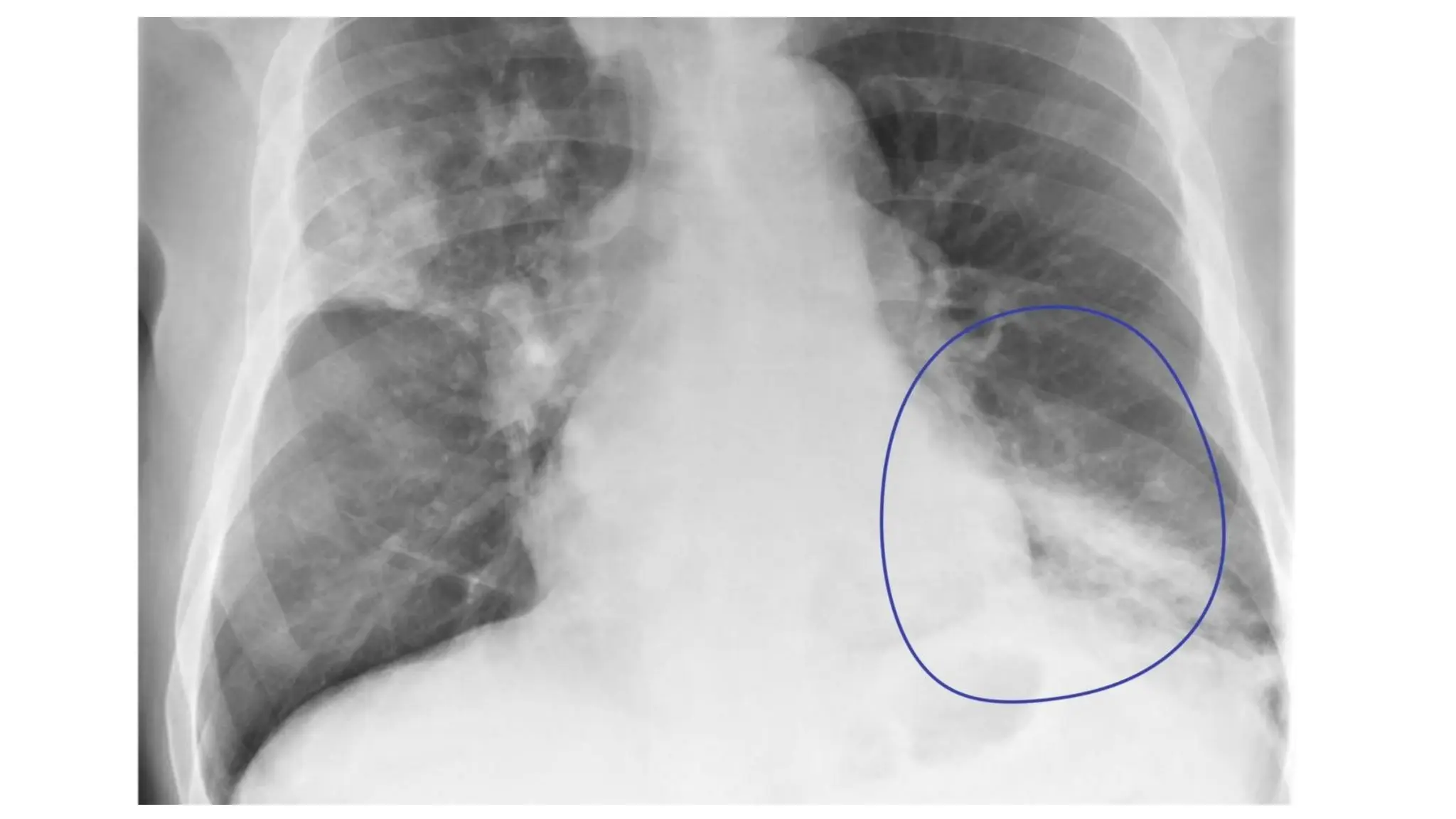
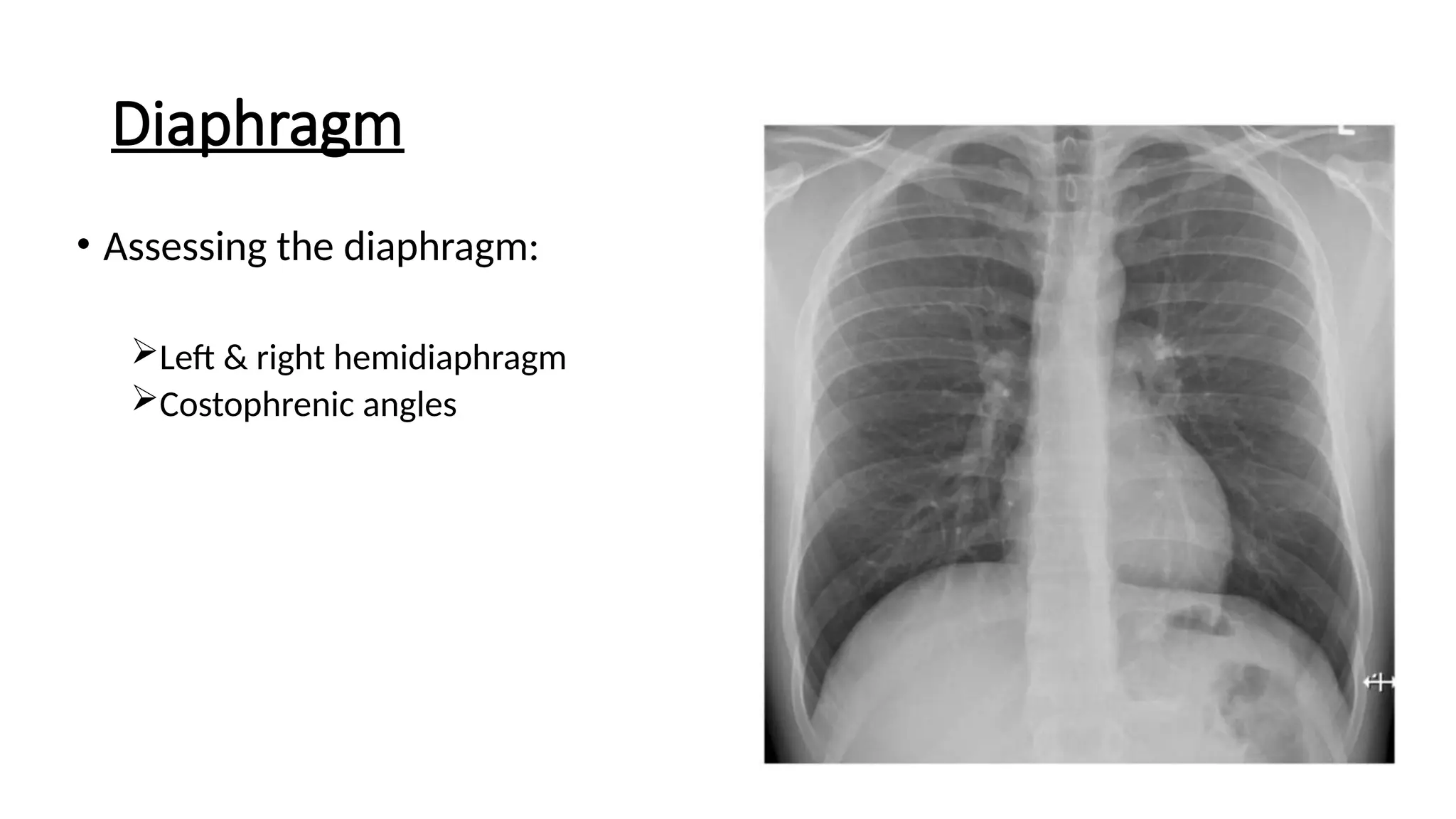
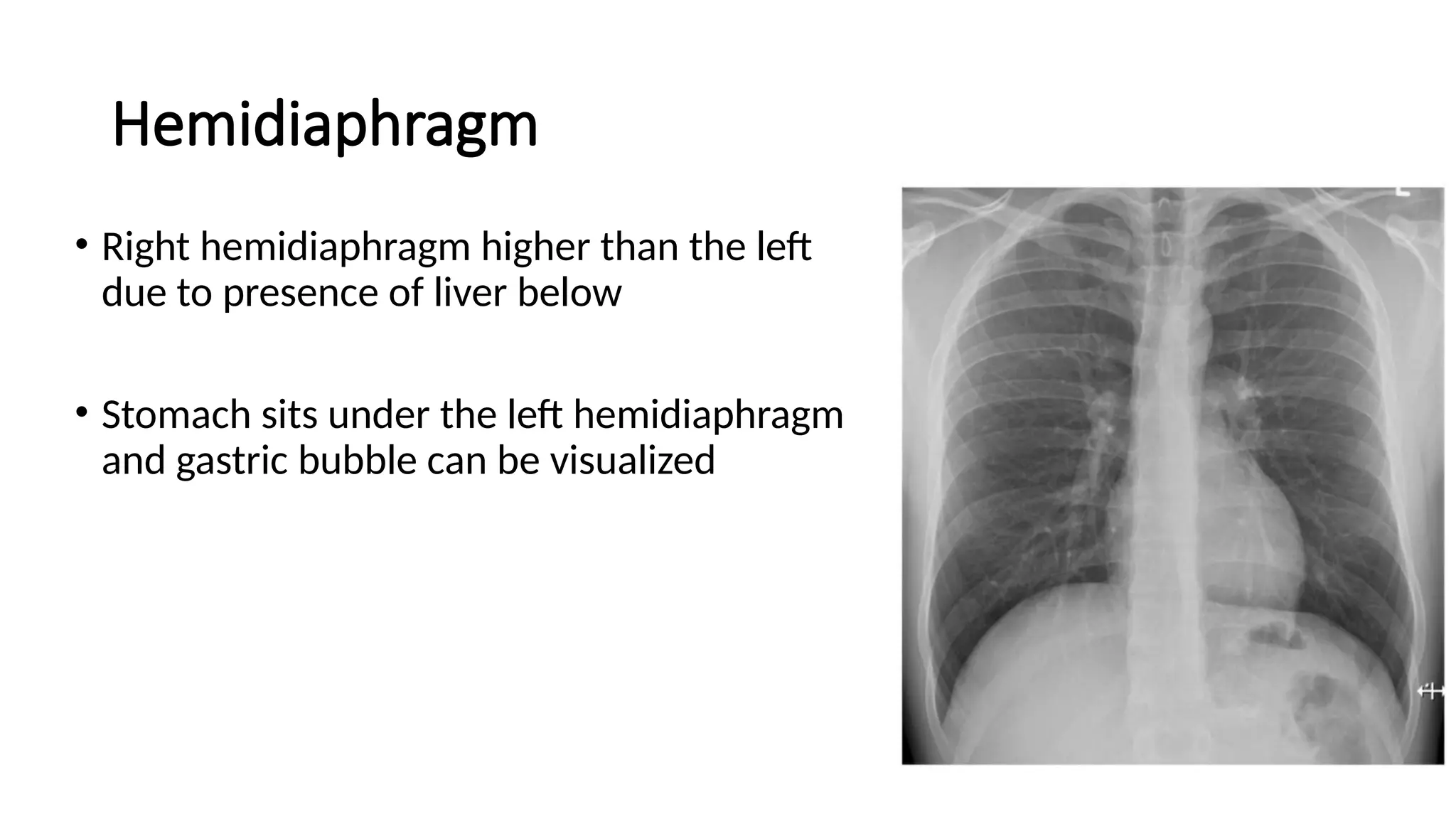
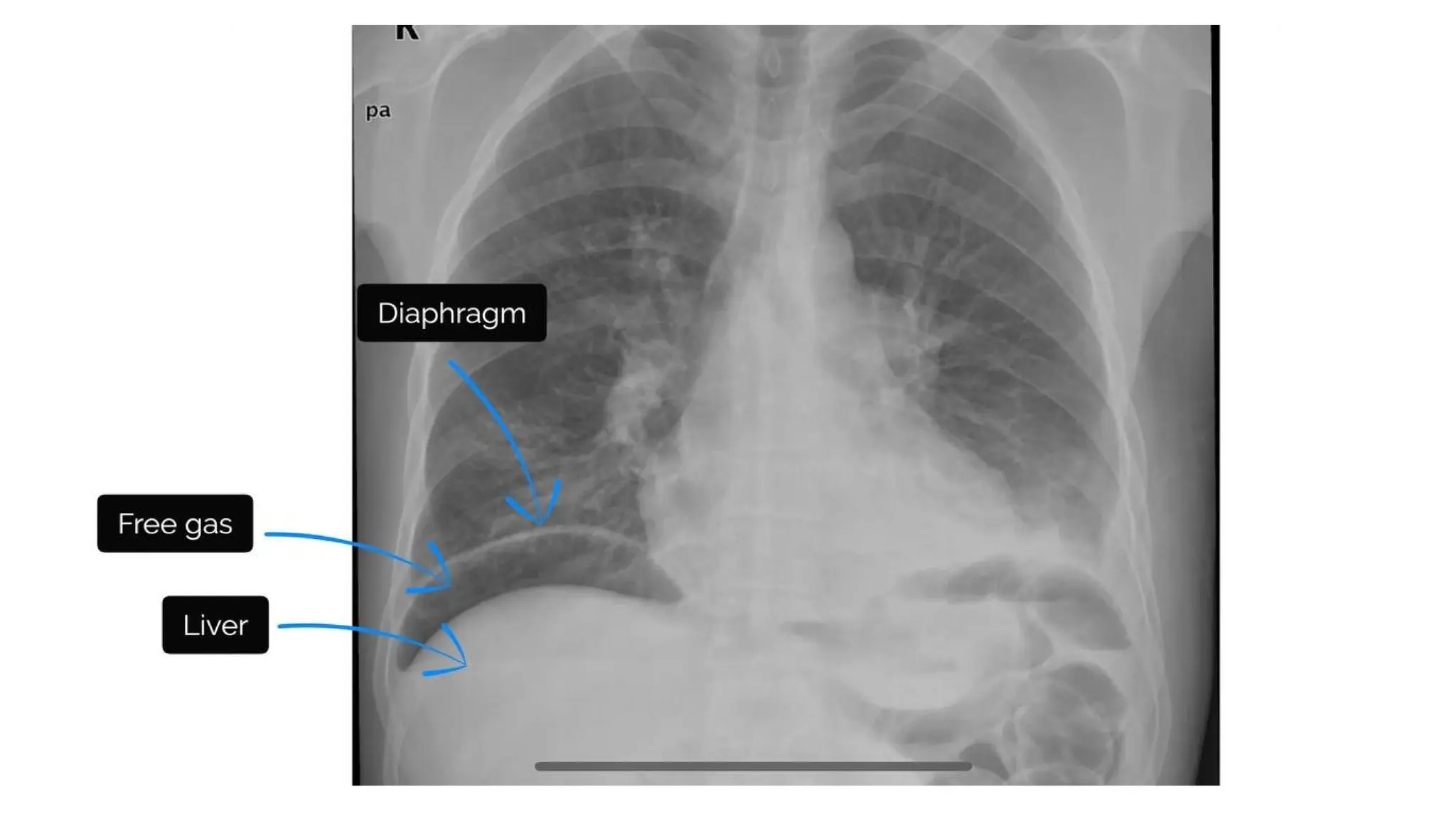
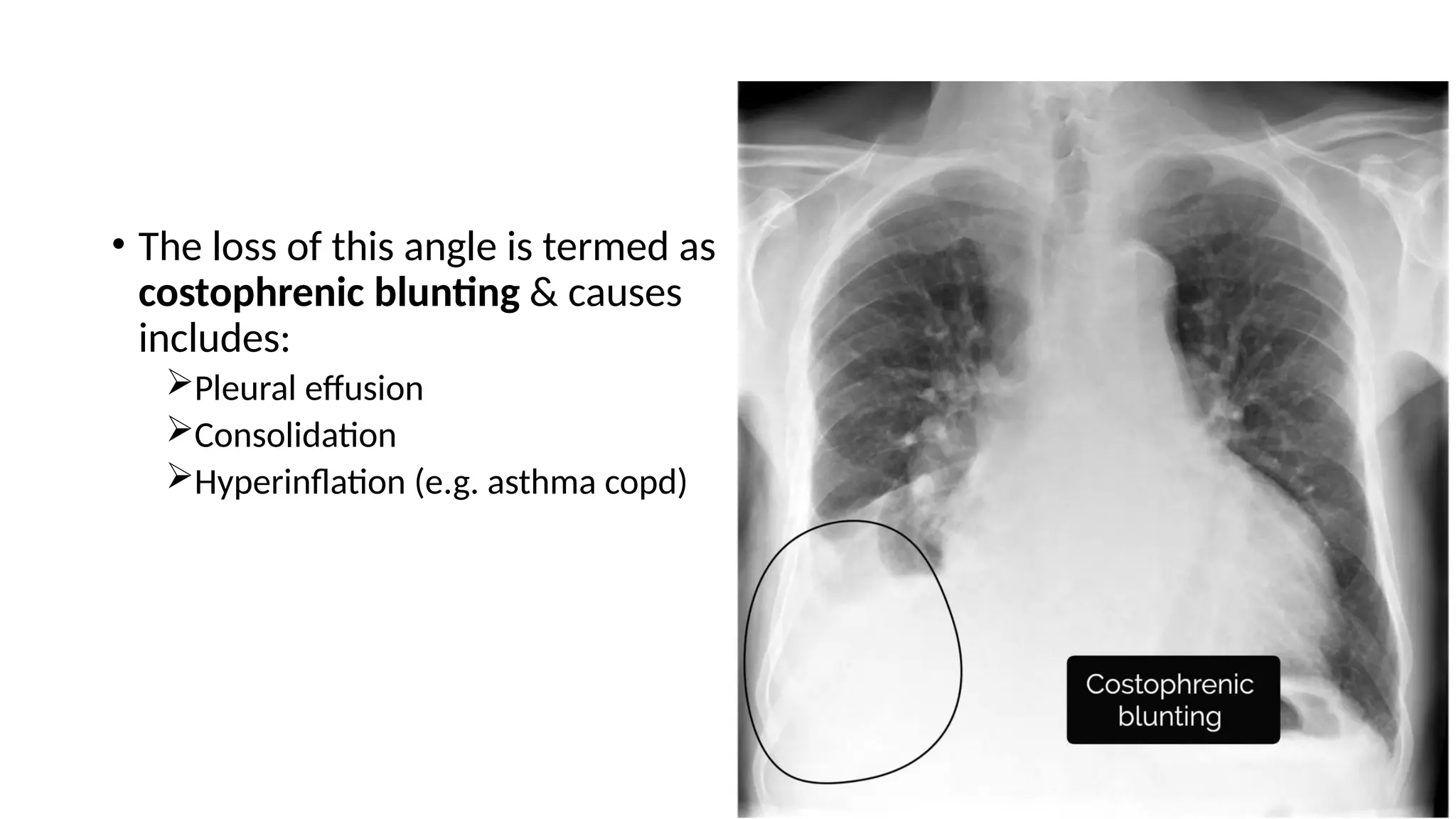
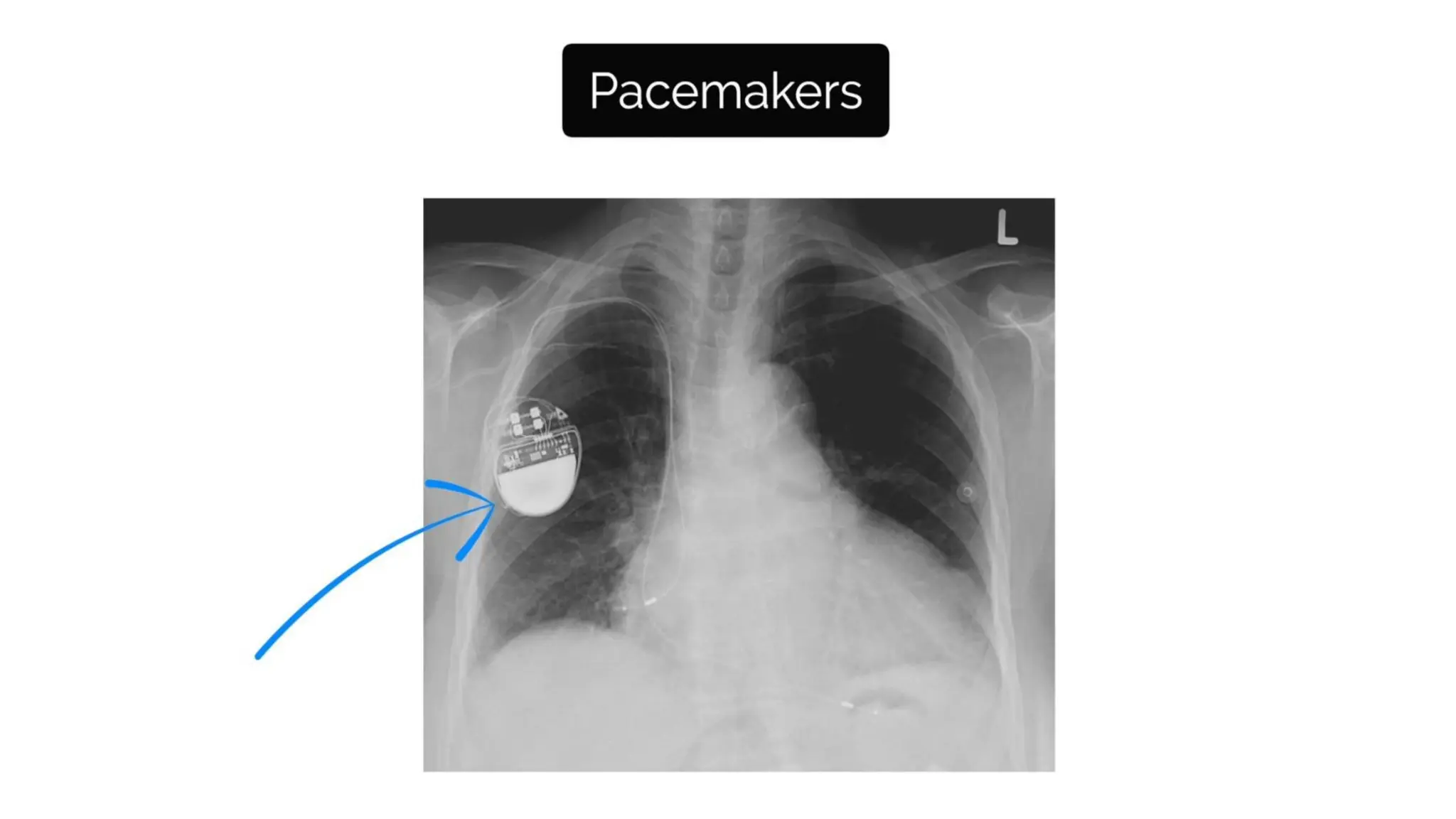
This document is a presentation on interpreting chest X-rays, covering fundamental principles, image quality assessment, and a systematic ABCDE approach to evaluation. Key factors include proper patient positioning, exposure quality, and recognizing pathologies like pulmonary edema and pneumothorax. It emphasizes the importance of documenting findings accurately and understanding clinical context for effective diagnosis.