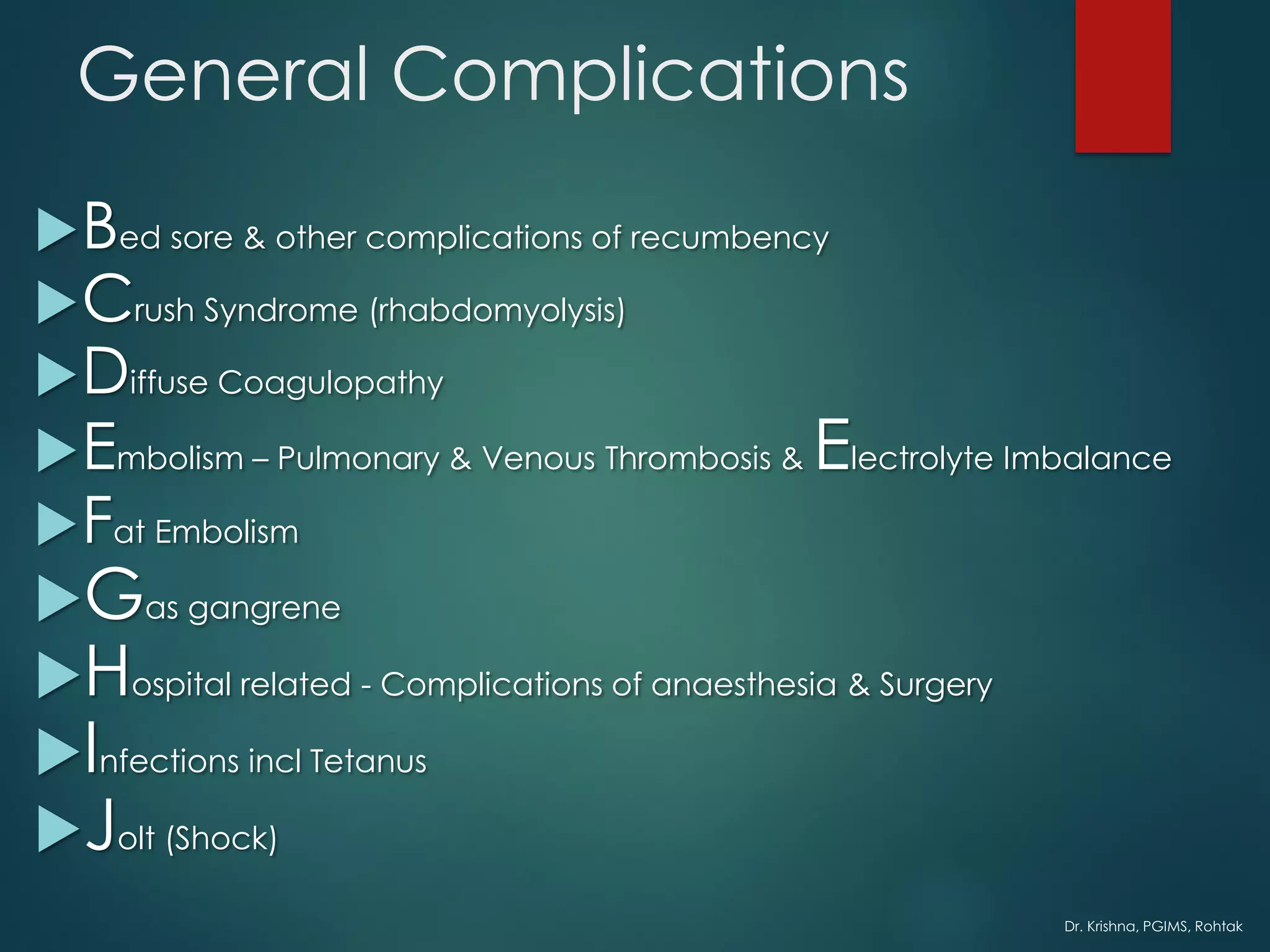
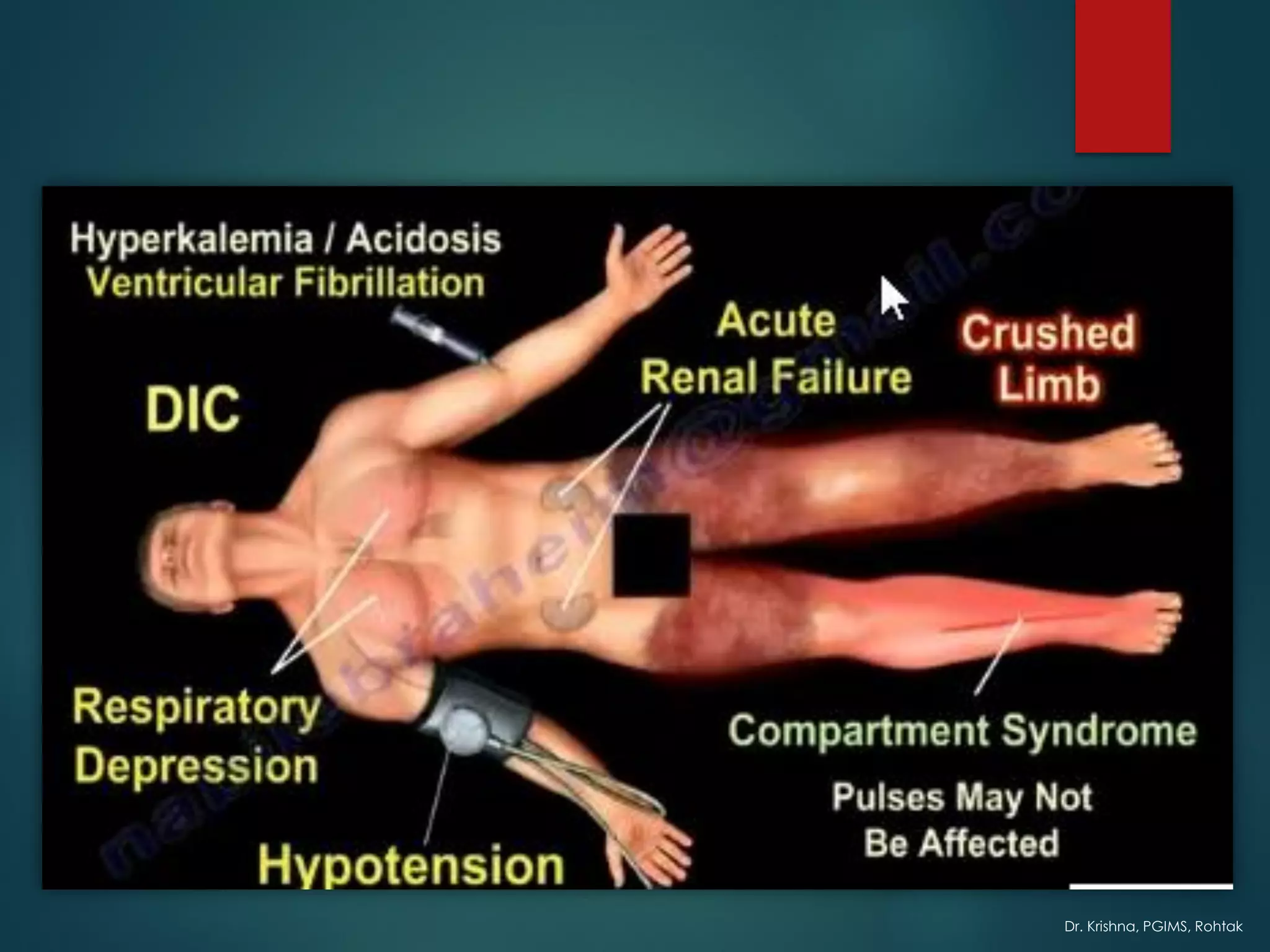
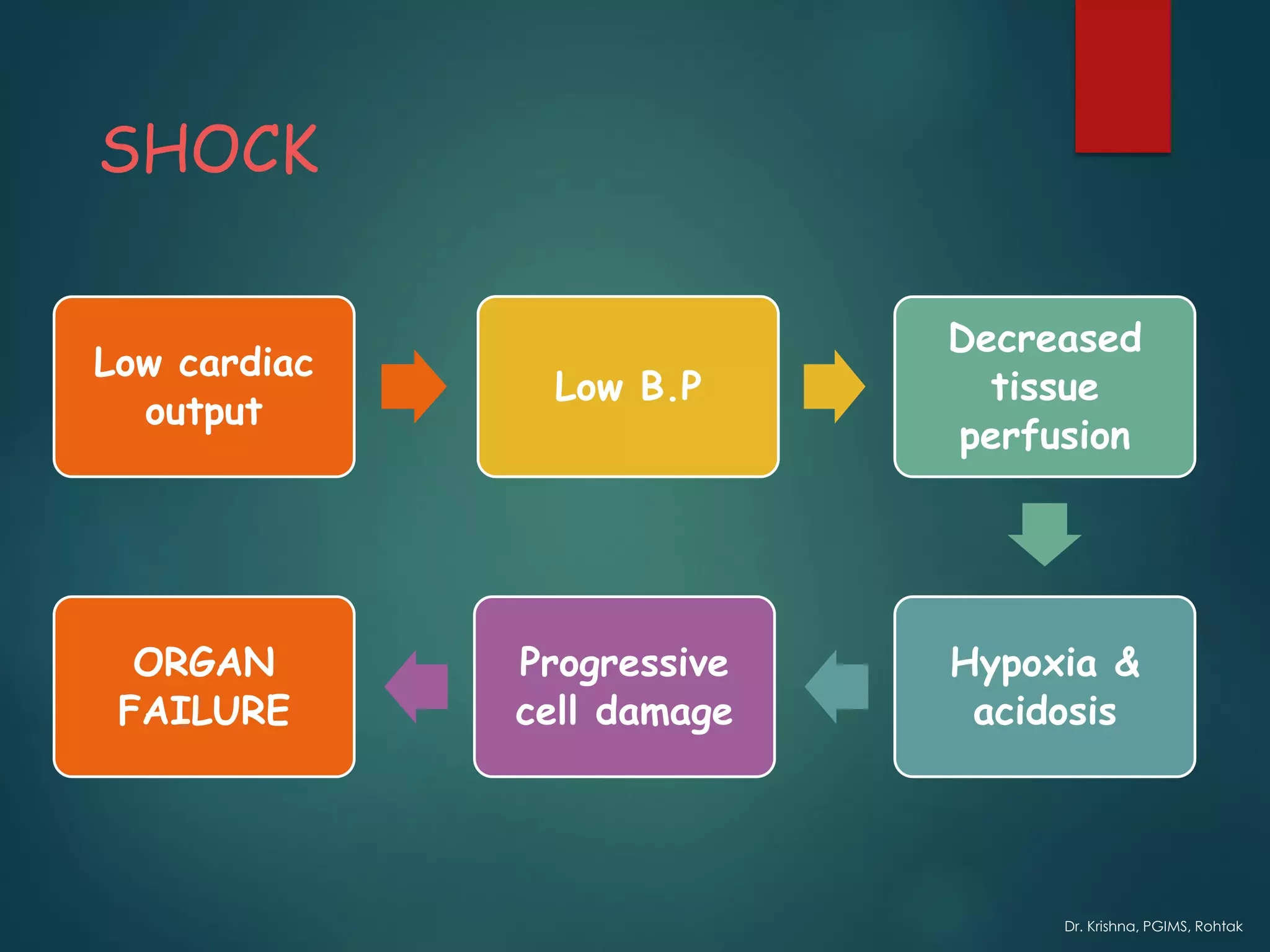
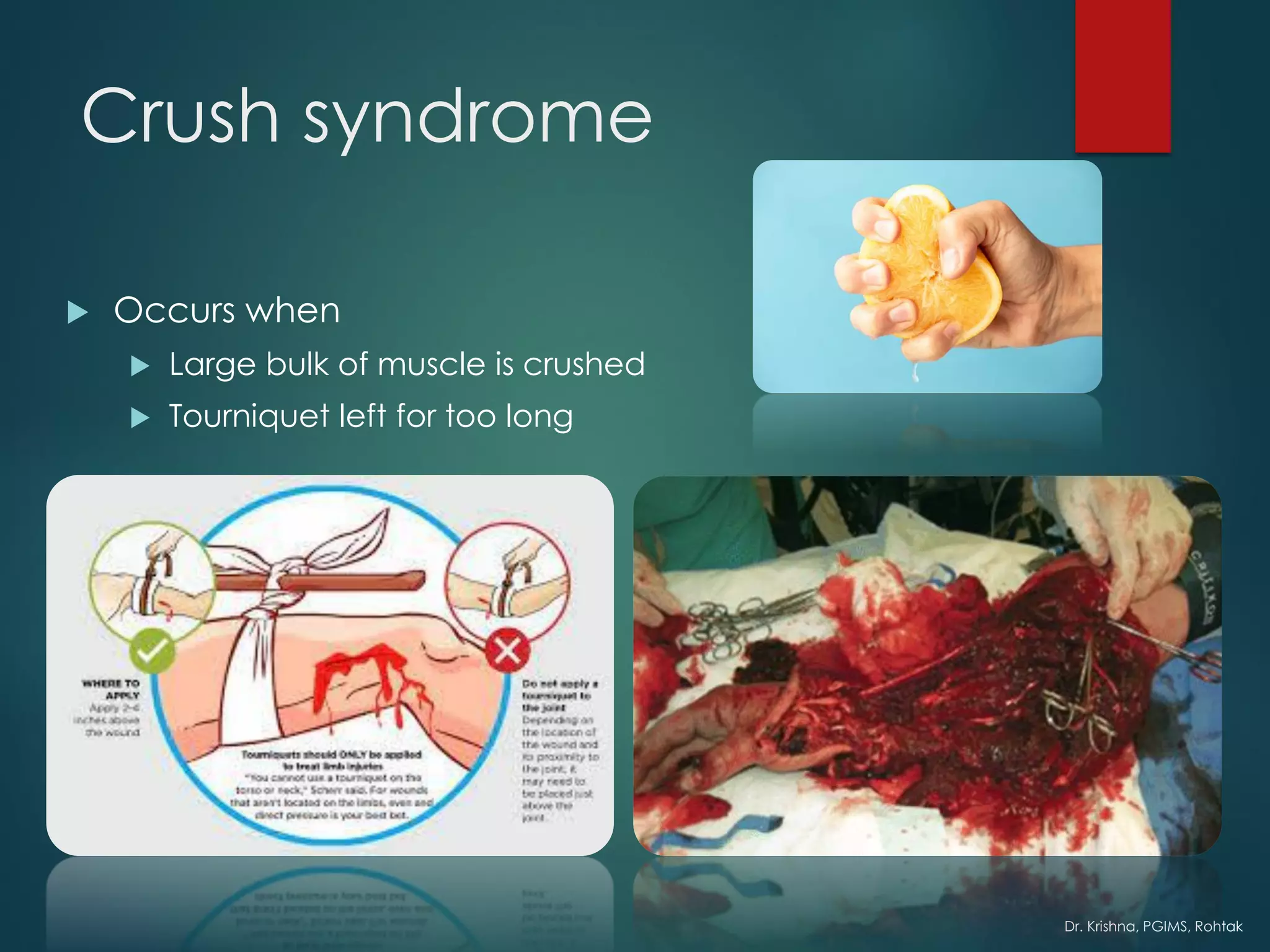
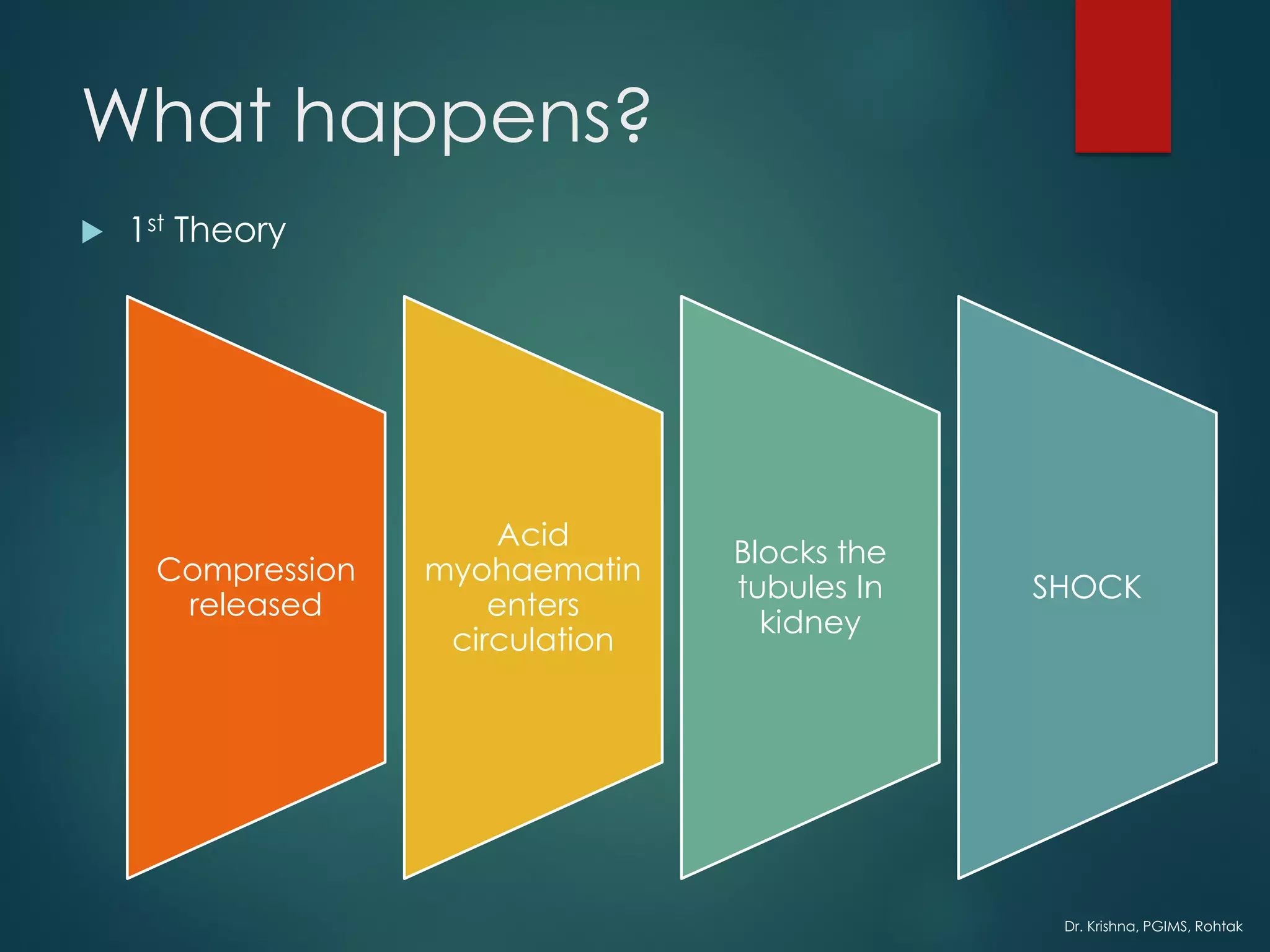
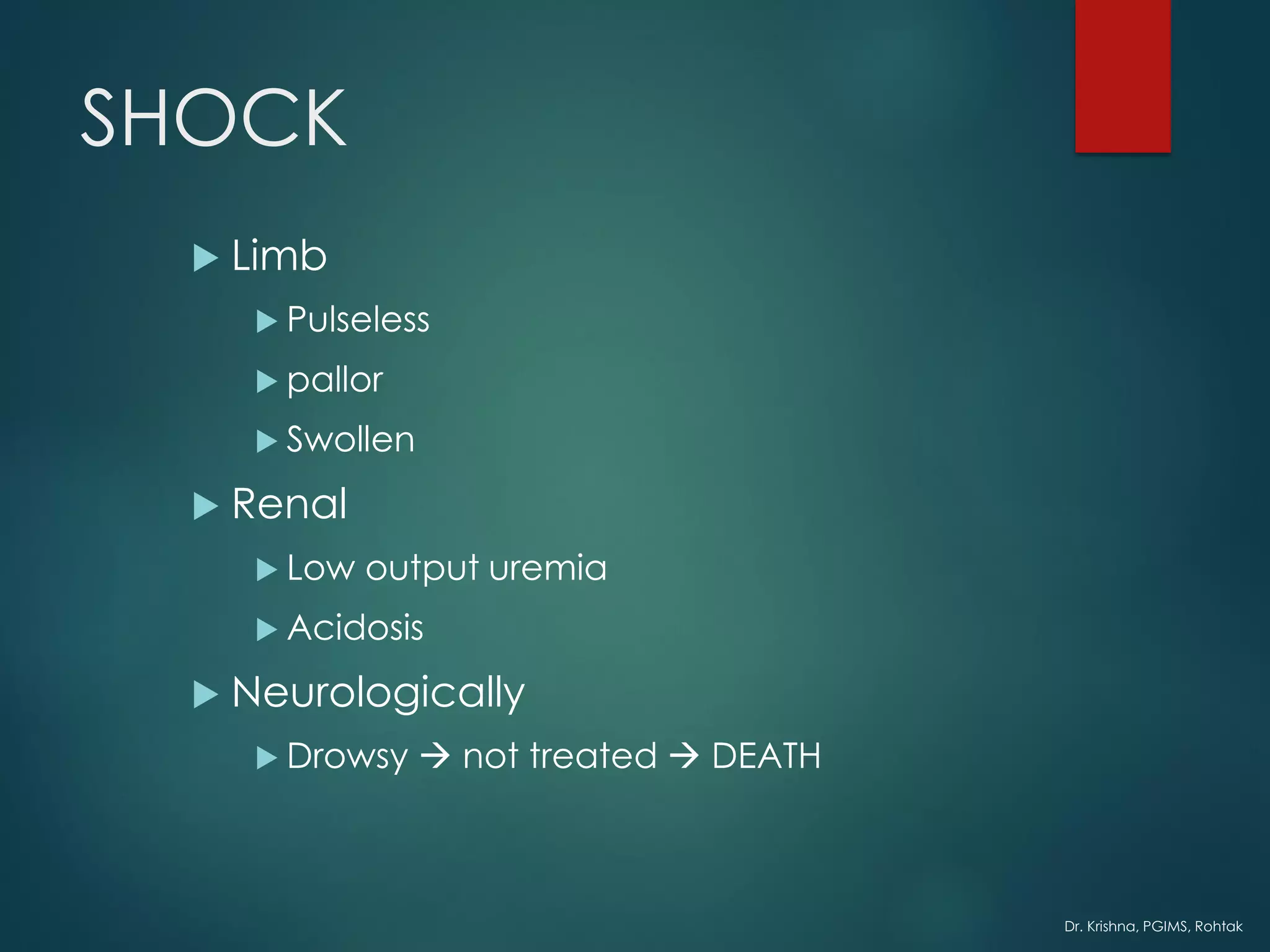
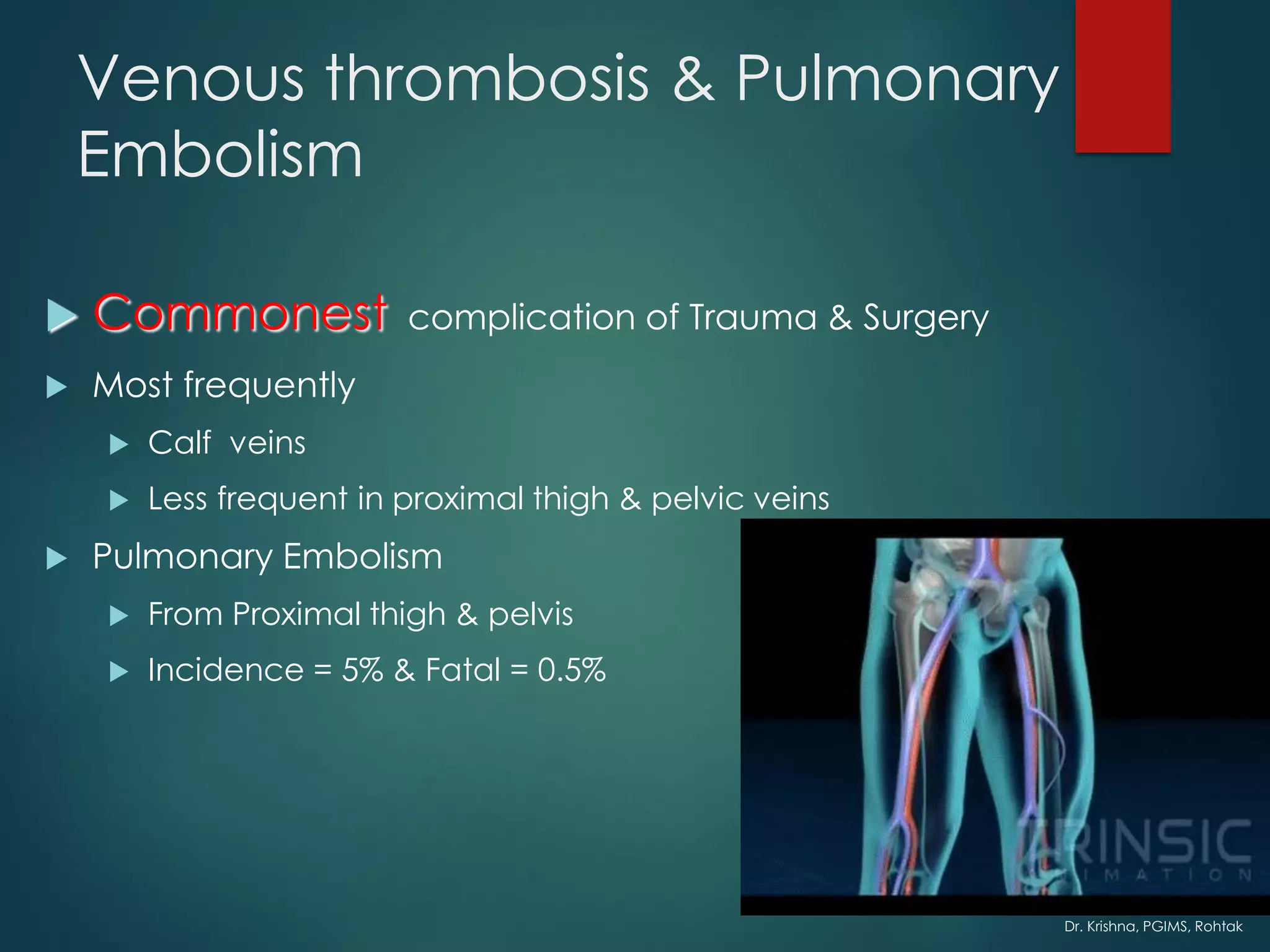
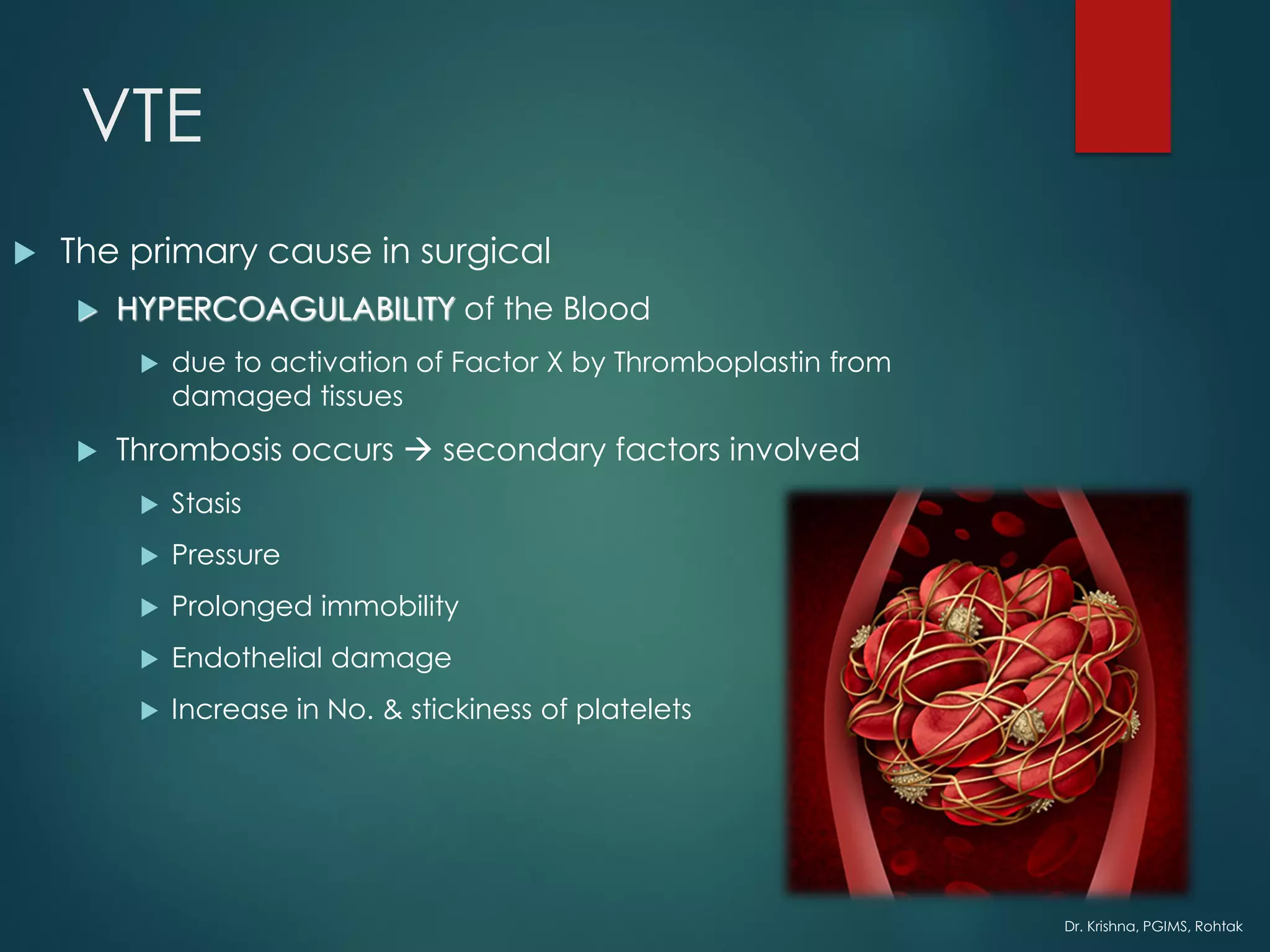
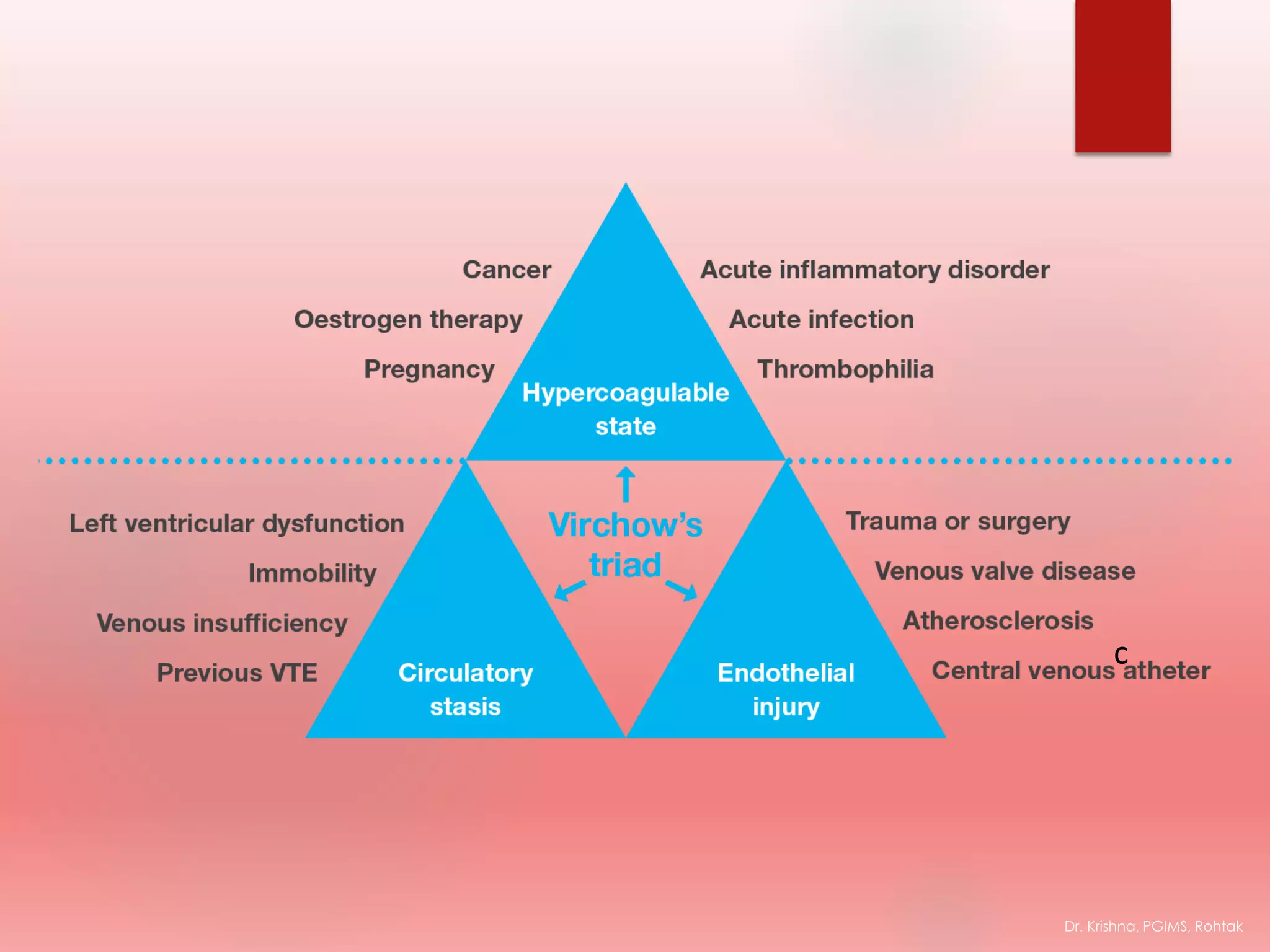
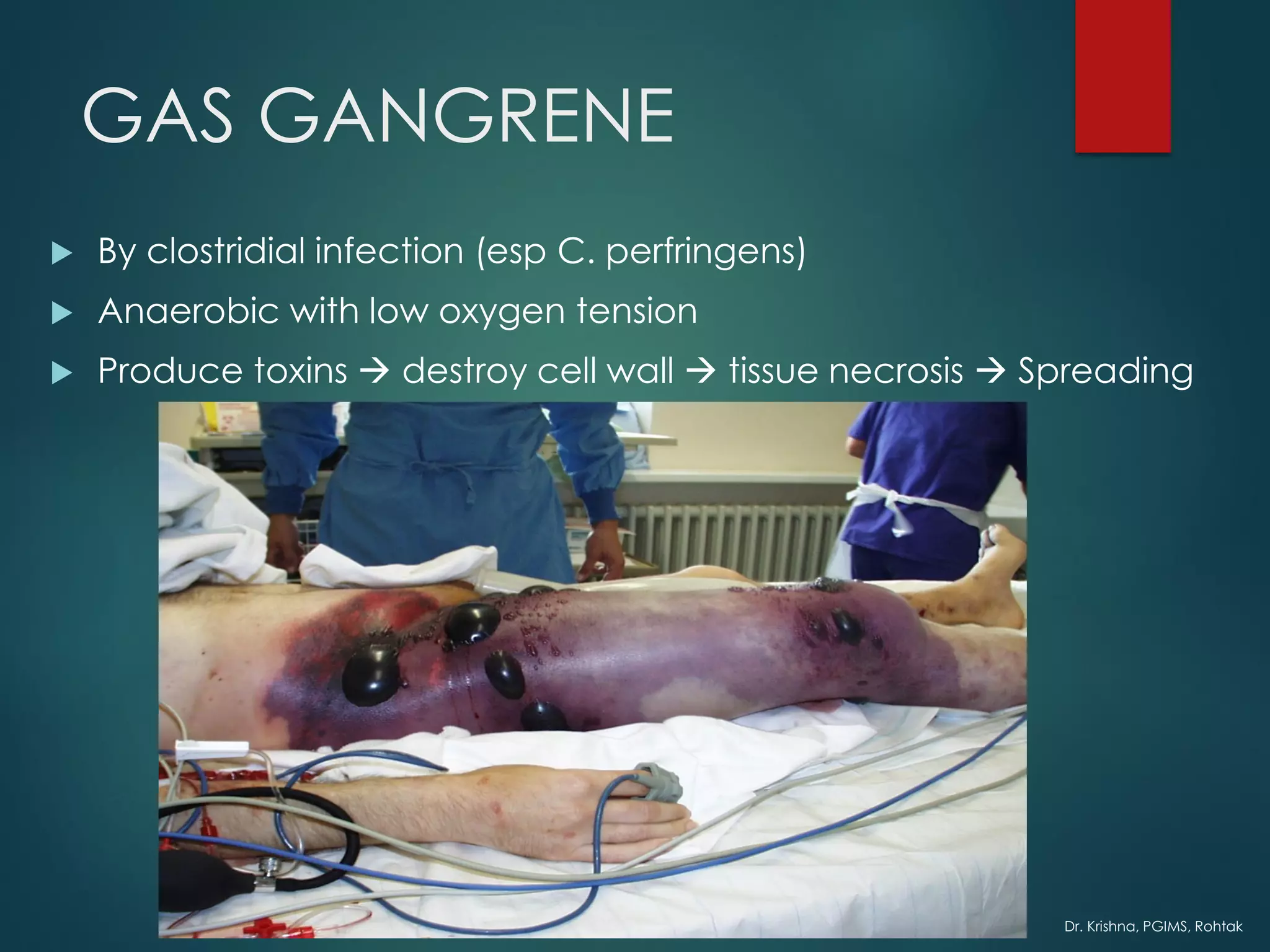
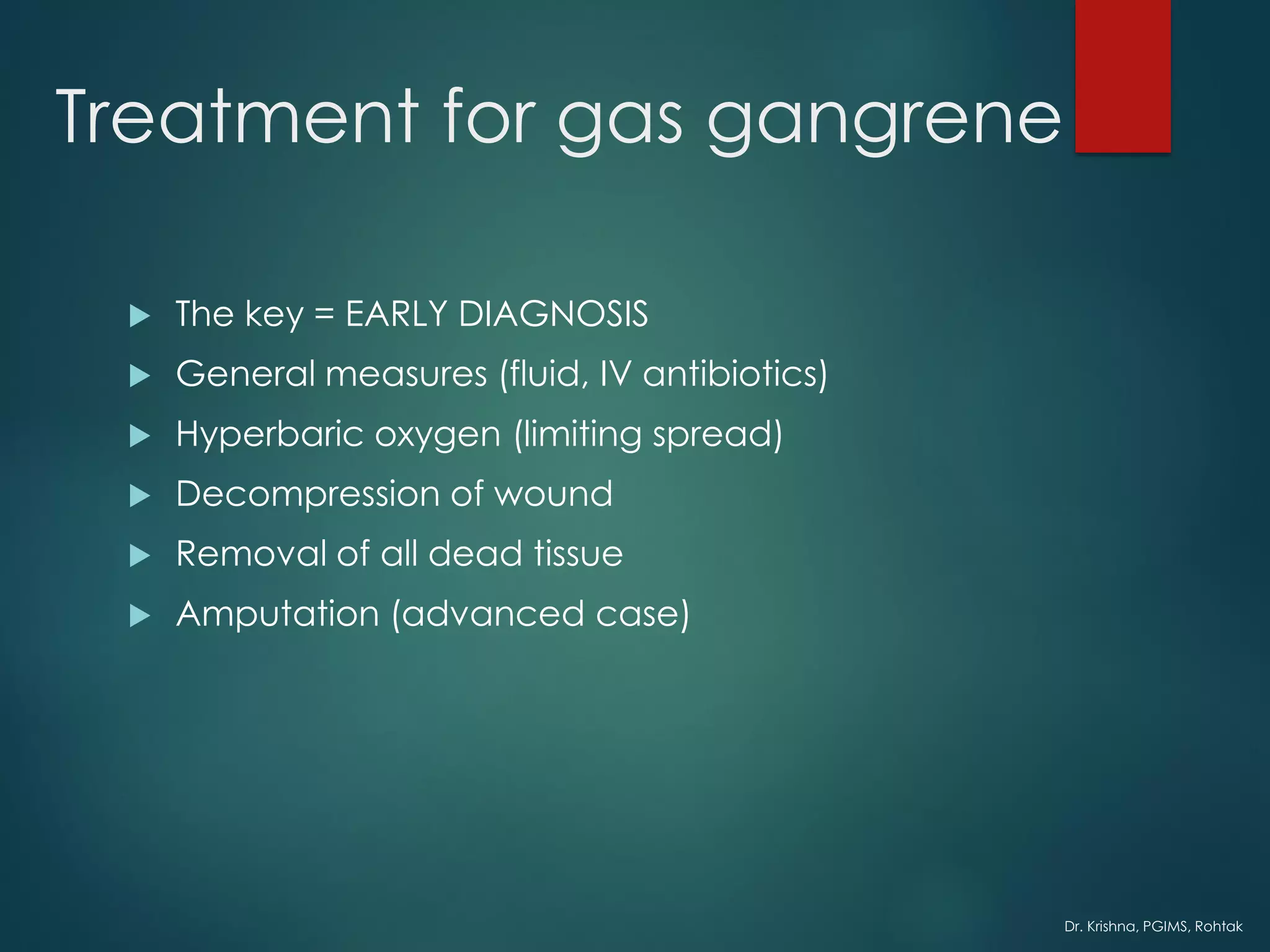
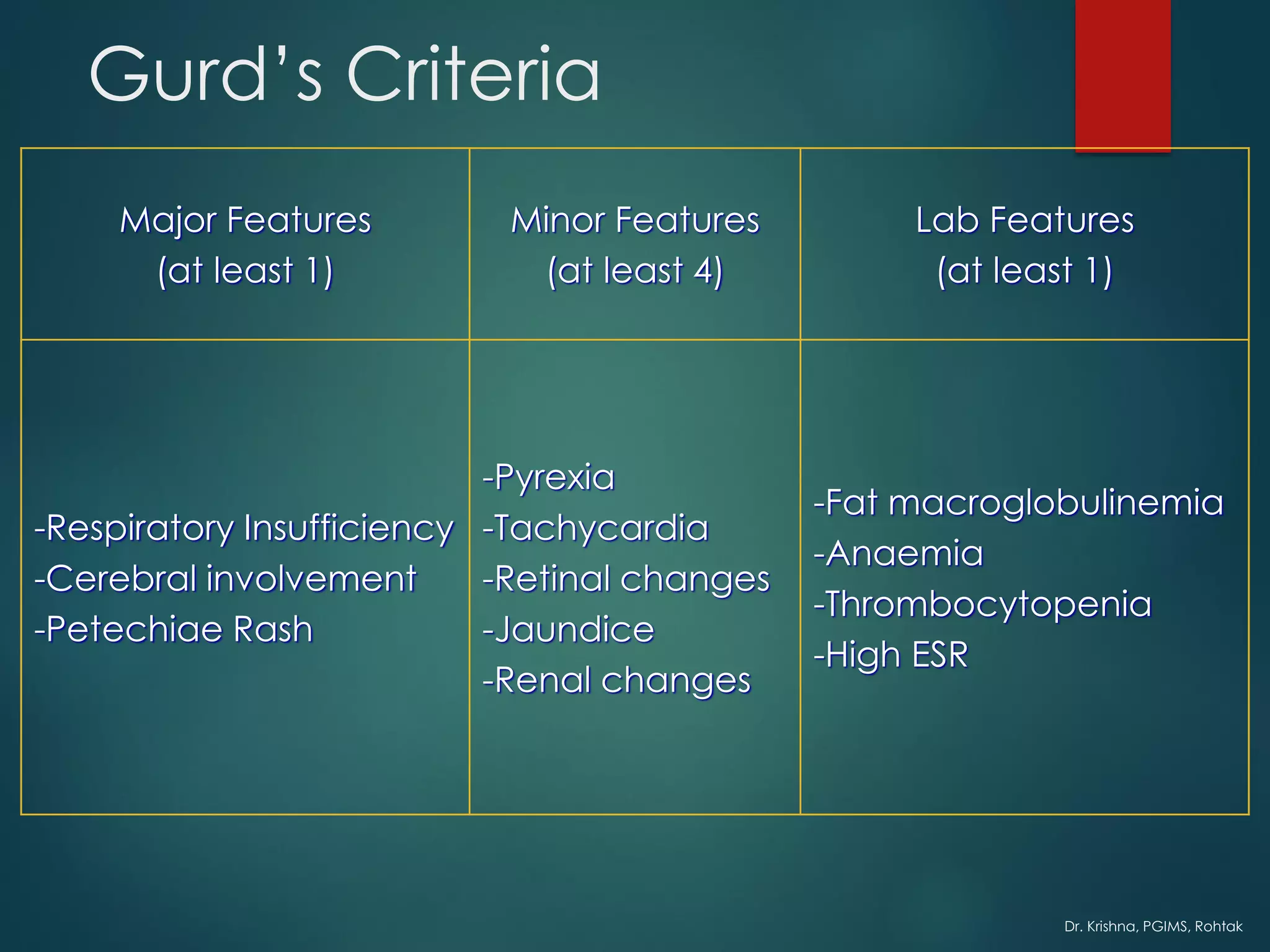
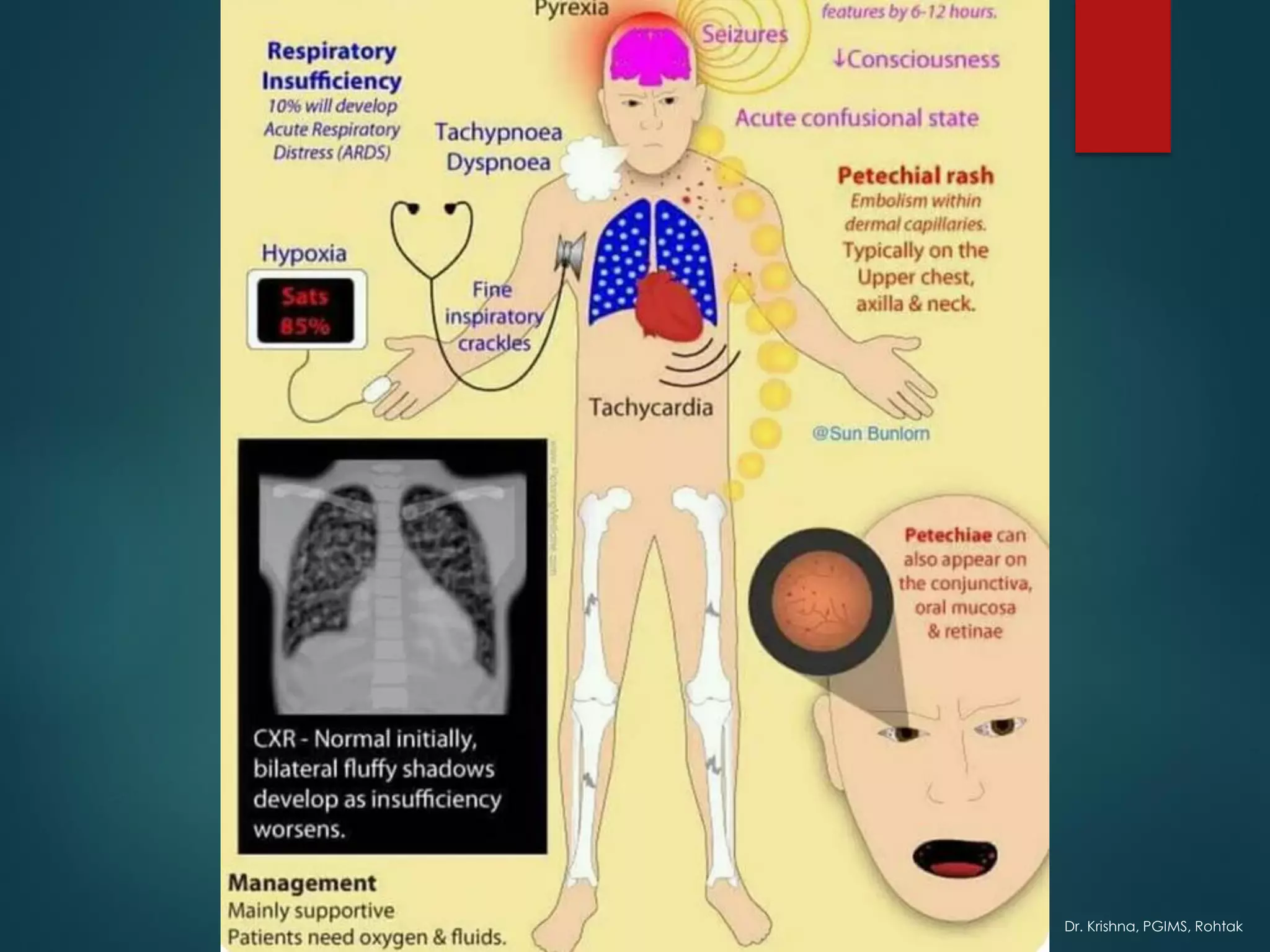
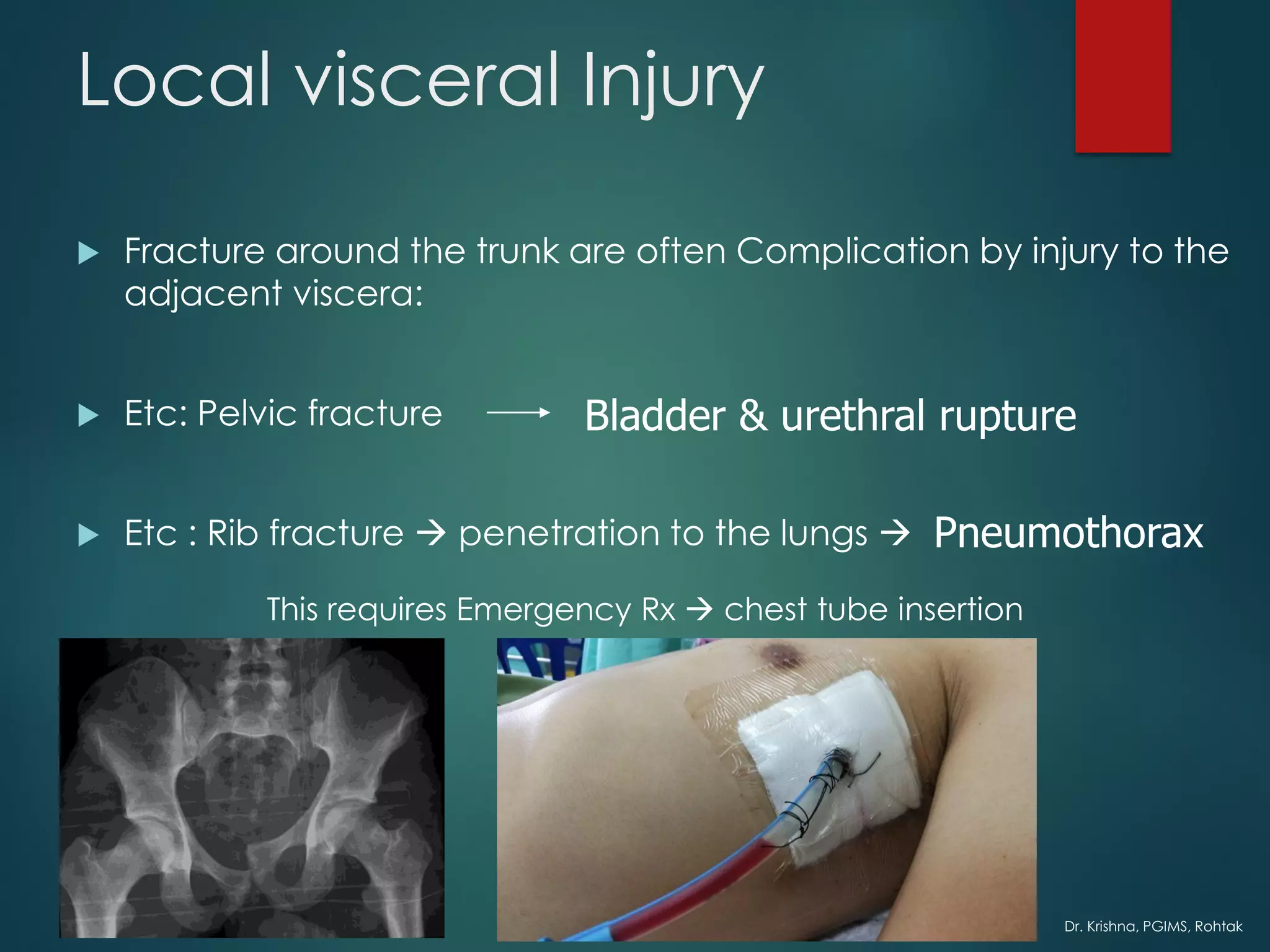
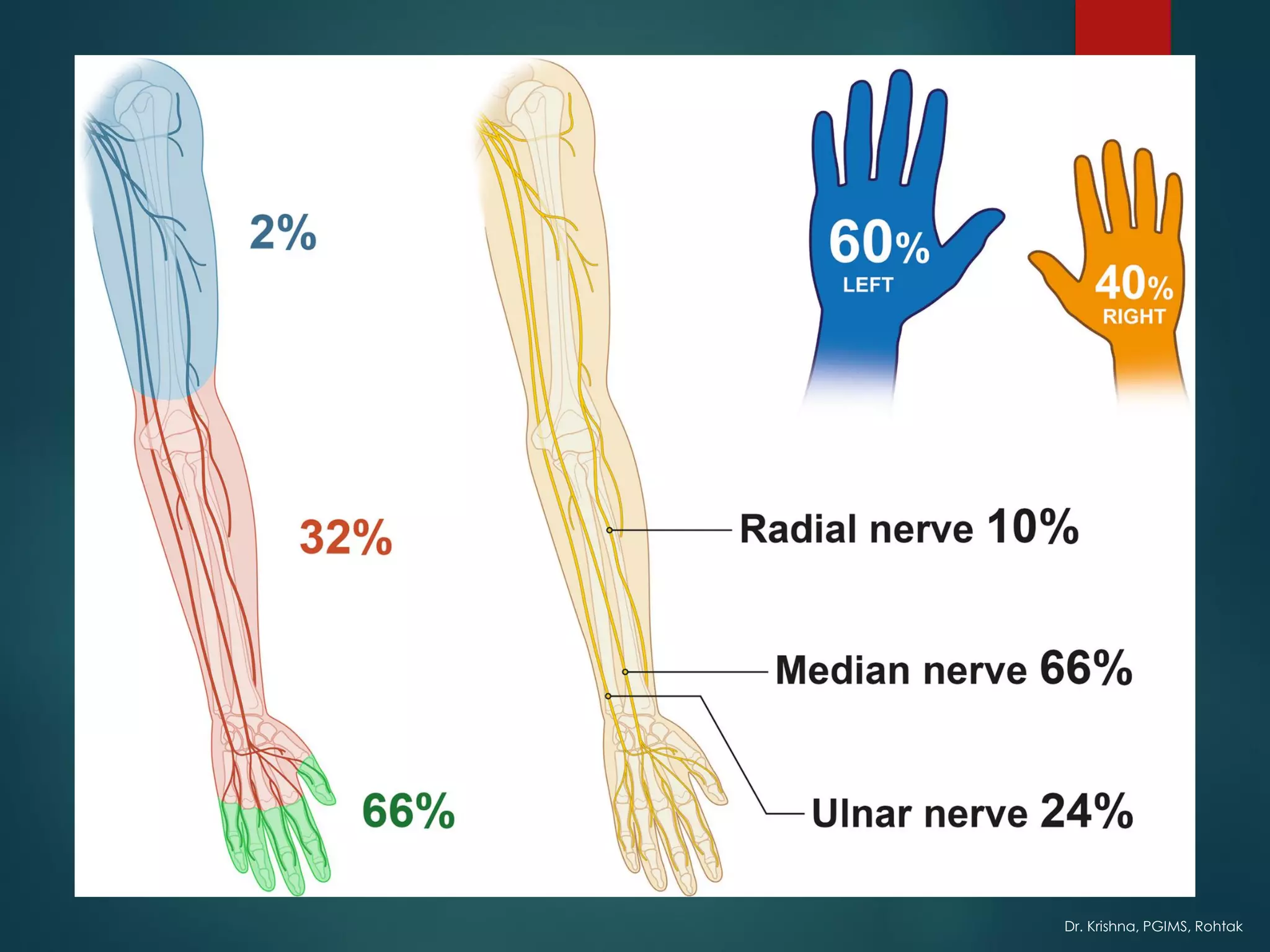
The document discusses various complications that can arise from fractures, including general complications like shock, crush syndrome, fat embolism, gas gangrene, and tetanus. It also discusses local complications like vascular injuries, nerve injuries, compartment syndrome, and infections. Early complications discussed include local visceral injuries, hemorrhage, and infections like gas gangrene, while late complications can include nonunion, malunion, arthritis, and osteomyelitis. Prevention and treatment approaches are provided for many of the complications.