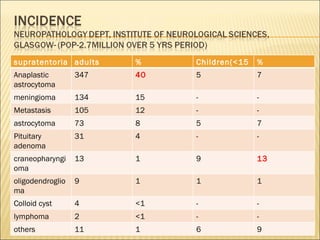
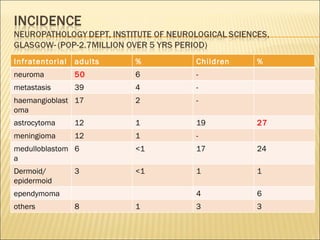
The document discusses brain tumors and their classification. It provides details about:
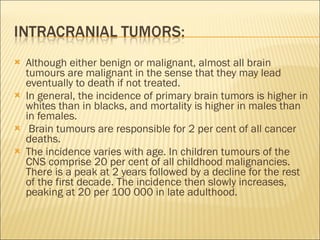
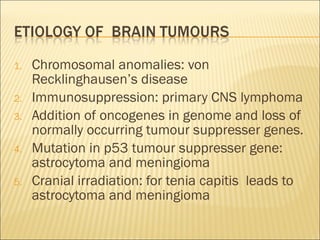
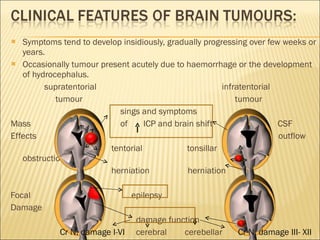
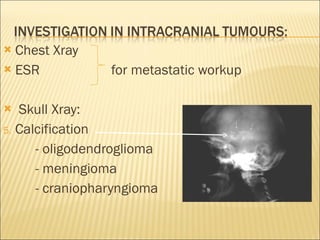
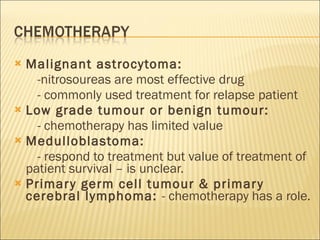
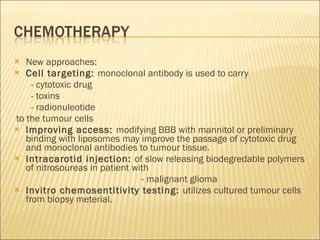
1) Primary brain tumors can arise from neurons, glia or meninges and metastases can spread from other organs. Prognosis depends on histology and location.
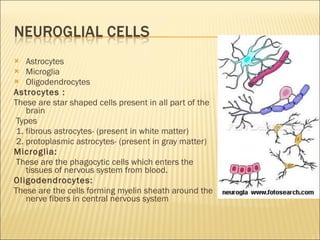
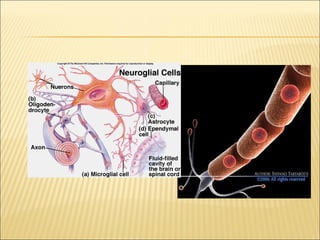
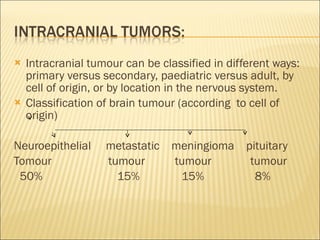
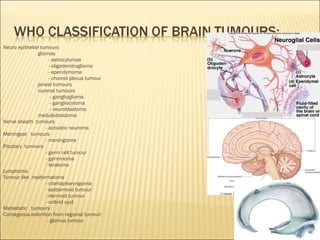
2) Brain tumors are classified based on their cell of origin - the majority are neuroepithelial tumors like gliomas and astrocytomas.
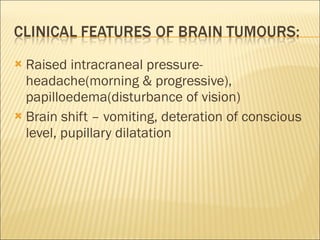
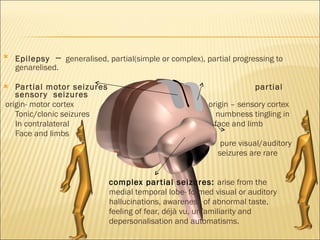
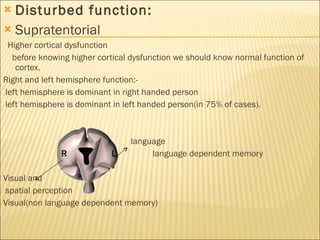
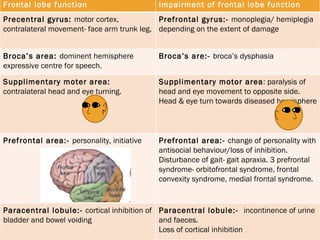
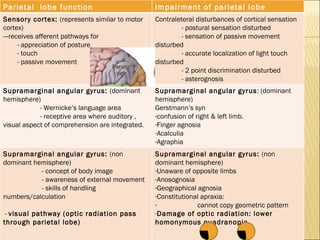
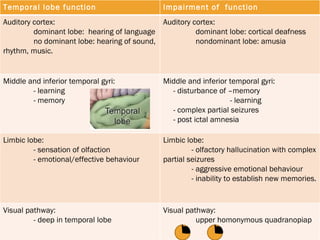
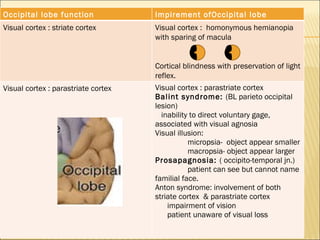
3) Symptoms vary based on tumor location but commonly include headaches, seizures, and neurological deficits.