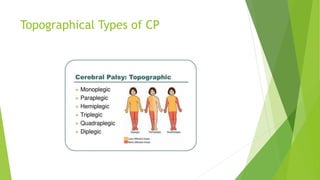
The document provides a comprehensive overview of cerebral palsy, including its history, neuroanatomy, causes, types, and the importance of early diagnosis and intervention. Key historical figures like Dr. William Little and Sir William Osler are highlighted for their contributions to understanding the condition. The text emphasizes the role of various diagnostic tools and the significance of early recognition to improve patient outcomes.



















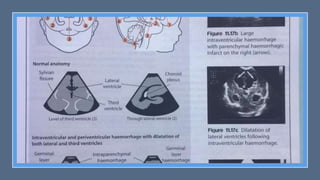
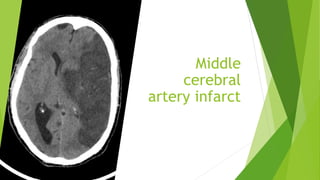
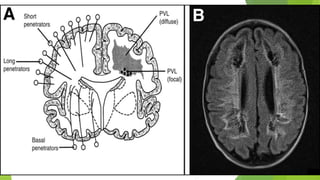
![MRI Brain
the literature suggests that MRI should be strongly considered in all cases; in
one study, 89% children with cerebral palsy were found to have abnormal
MRIs. [37] Additionally, MRI may have a role in predicting neurodevelopmental
outcomes in preterm infants. [38] See the following images.](https://image.slidesharecdn.com/cerebralpalsy-finalversionforslideshare2-231025043449-b2262f75/85/Cerebral-Palsy-84-320.jpg)


![Neurological criteria
Neurological criteria
One of the following:
The presence of seizures is an automatic inclusion
Evidence of encephalopathy suggested by amplitude-integrated EEG (a-EEG)
Physical examination consistent with moderate to severe encephalopathy [Table 2]
Table 2](https://image.slidesharecdn.com/cerebralpalsy-finalversionforslideshare2-231025043449-b2262f75/85/Cerebral-Palsy-92-320.jpg)
















![Early markers
for CP
There are several neurological
examination methods available for
high-risk infants used for both clinical
care and research studies. The well-
known methods are the Hammersmith
Infant Neurological Examination (HINE)
[50], the Touwen [51], the Amiel-Tison
[52], the Bayley Scales of Infant and
Toddler Development [53], and
Dubowitz neonatal neurological
examination [54].](https://image.slidesharecdn.com/cerebralpalsy-finalversionforslideshare2-231025043449-b2262f75/85/Cerebral-Palsy-142-320.jpg)











![Early markers
for CP
These assessment methods have a high
predictive value with sensitivity and
specificity of 88 and 92%, respectively,
in predicting CP [14]. The use of the
above neuromotor and developmental
assessment is to predict impairments as
early as possible and to help physician
provide guidance for families about
their children development and help in
discriminating between normally
developing infants from those with
abnormal development. It also enables
prognostic information on the
neurological and motor outcome and
when to send those infants showing
early impairment for rehabilitation
programs](https://image.slidesharecdn.com/cerebralpalsy-finalversionforslideshare2-231025043449-b2262f75/85/Cerebral-Palsy-166-320.jpg)
![HINE
It consists of 26 items that assess
different aspects of neurological
examinations such as cranial nerves,
posture, movements, tone, and
reflexes [53], with a questionnaire
instructions and diagrams included on
the scoring sheet, similar to Dubowitz
neonatal neurological examinations
[54]. Each item is scored individually
(0, 1, 2, or 3), with a sum score of all
individual items (range 0–78),
Optimality scores for infants 3 to 18
months are based on the frequency of
distribution of neurological findings in
a typical infant population: it is
considered optimal when an item is
found in at least 90% of infants [53].](https://image.slidesharecdn.com/cerebralpalsy-finalversionforslideshare2-231025043449-b2262f75/85/Cerebral-Palsy-168-320.jpg)
![HINE
The sequential use of the HINE allows the identification of early signs of
cerebral palsy and other neuromotor disorders, while individual items are
predictive of motor outcomes. For example, in preterm infants assessed
between 6 and 15 months of corrected age, scores above 64 predict
independent walking with a walked sensitivity of 98% and specificity of 85%.
Conversely, scores below 52 were highly predictive of cerebral palsy and
severe motor impairments [55].](https://image.slidesharecdn.com/cerebralpalsy-finalversionforslideshare2-231025043449-b2262f75/85/Cerebral-Palsy-169-320.jpg)
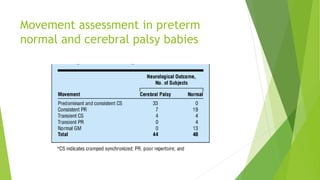
![General Movements
It is characterized by a movement that involves the whole body in a variable
sequence involving the arm, leg, neck, and trunk. They are complex in nature
that wax, and wane vary in intensity, speed, and range of motion and have a
gradual onset and end. It has been proposed that GMs consist of rhythmic
bursts of action potentials [16]. GMs are generated from a large neuronal
generator network that extends from the brain stem to the spinal cord [25].](https://image.slidesharecdn.com/cerebralpalsy-finalversionforslideshare2-231025043449-b2262f75/85/Cerebral-Palsy-171-320.jpg)





![Risk facors Risk factors — In addition to prematurity and BW,
which are important risk factors for developing CP,
numerous other prenatal and perinatal risk factors
have been reported (table 1), though for many of
these risk factors, a causal relationship has not been
established [2,7-12]. Potentially modifiable prenatal
factors that may contribute to CP risk include heavy
maternal alcohol consumption, maternal smoking,
maternal obesity, and infections during pregnancy
[13-17]. CP is most often multifactorial, and multiple
risk factors coexist. (](https://image.slidesharecdn.com/cerebralpalsy-finalversionforslideshare2-231025043449-b2262f75/85/Cerebral-Palsy-194-320.jpg)
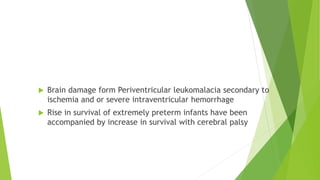
![Trends over
time
Trends over time — In the 1960s through 1980s, the
rate of CP and the extent of disability among
preterm infants increased as survival improved for
the most premature [18]. During the 1980s and
1990s, there was a reversal in this trend, most likely
because of improvements in perinatal care. In one
study, the prevalence of CP among very low birth
weight (VLBW; <1500 g) infants declined from 60.6
per 1000 live births in 1980 to 39.5 per 1000 live
births in 1996 [19]. [21].](https://image.slidesharecdn.com/cerebralpalsy-finalversionforslideshare2-231025043449-b2262f75/85/Cerebral-Palsy-195-320.jpg)
![ This improvement occurred despite overall increases in survival and multiple
births and decreases in mean BW among this group. In another study, the
prevalence of CP among preterm infants (GA 20 to 27 weeks) decreased from
155 per 1000 live births in the early 1990s (1992 to 1994) to 16 per 1000 live
births in the early 2000s (2001 to 2003) [20]. This was in the setting of stable
or decreasing mortality during the same time period.
Among term and late preterm infants, the prevalence of CP remained stable
during the 1980s and 1990s](https://image.slidesharecdn.com/cerebralpalsy-finalversionforslideshare2-231025043449-b2262f75/85/Cerebral-Palsy-196-320.jpg)
![Multifactorial AETILOGY
The multifactorial etiology of CP was illustrated in a series of 213 children
diagnosed with CP in Australia, of whom 98 percent had contributing causes
other than intrapartum hypoxia [24]. The relative frequencies of different
contributing causes was as follows (many children had more than one cause)](https://image.slidesharecdn.com/cerebralpalsy-finalversionforslideshare2-231025043449-b2262f75/85/Cerebral-Palsy-197-320.jpg)