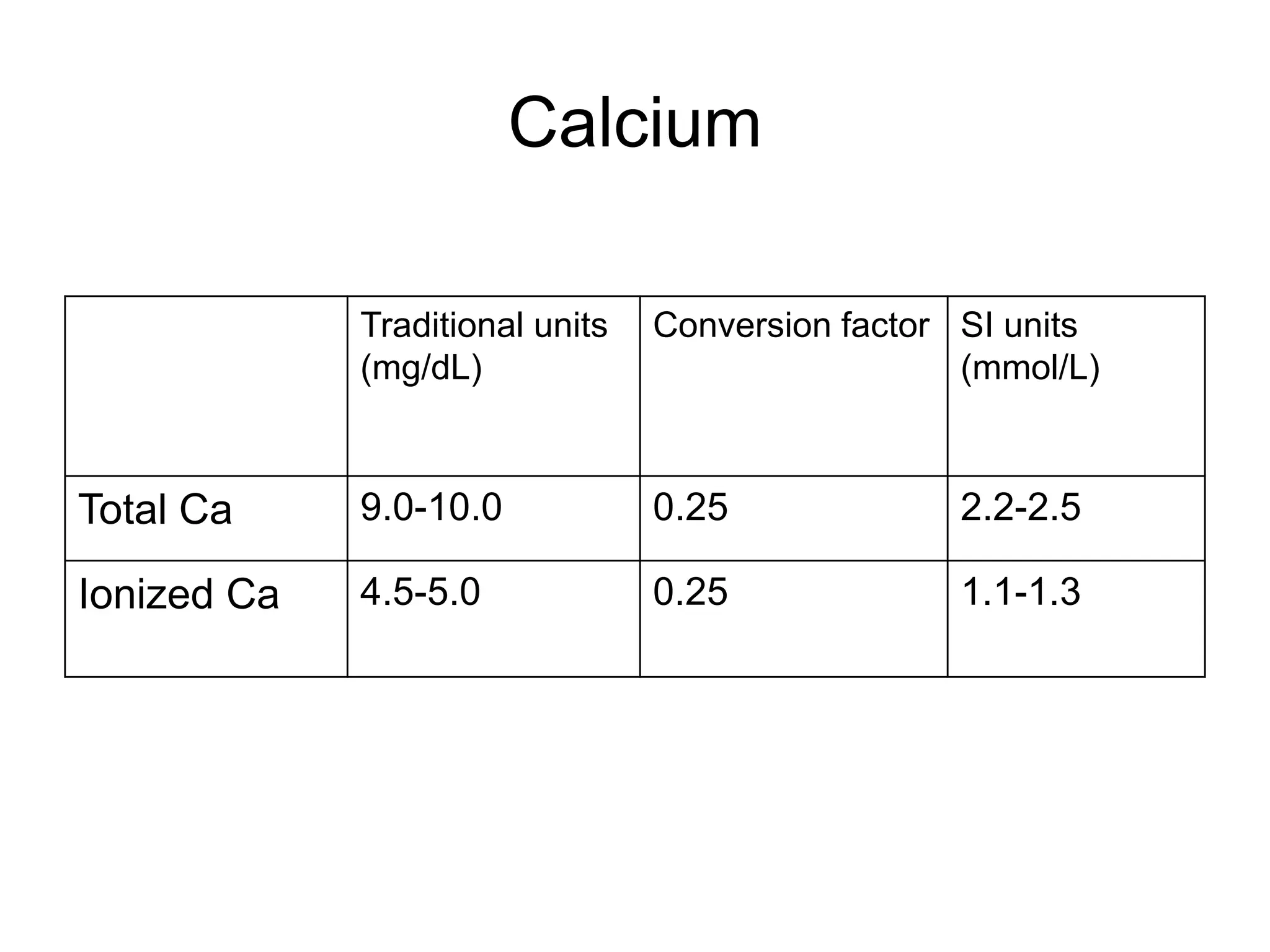
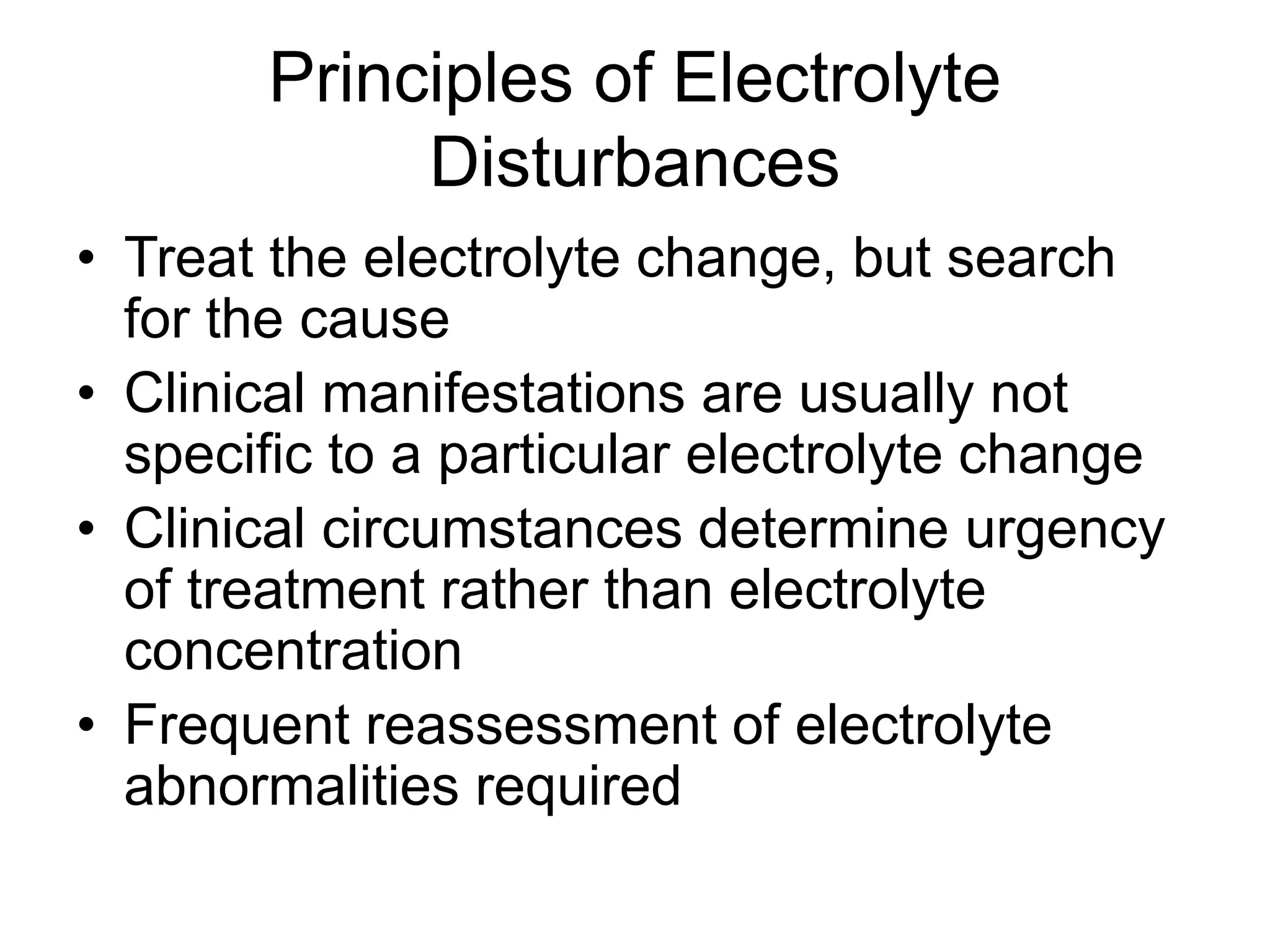
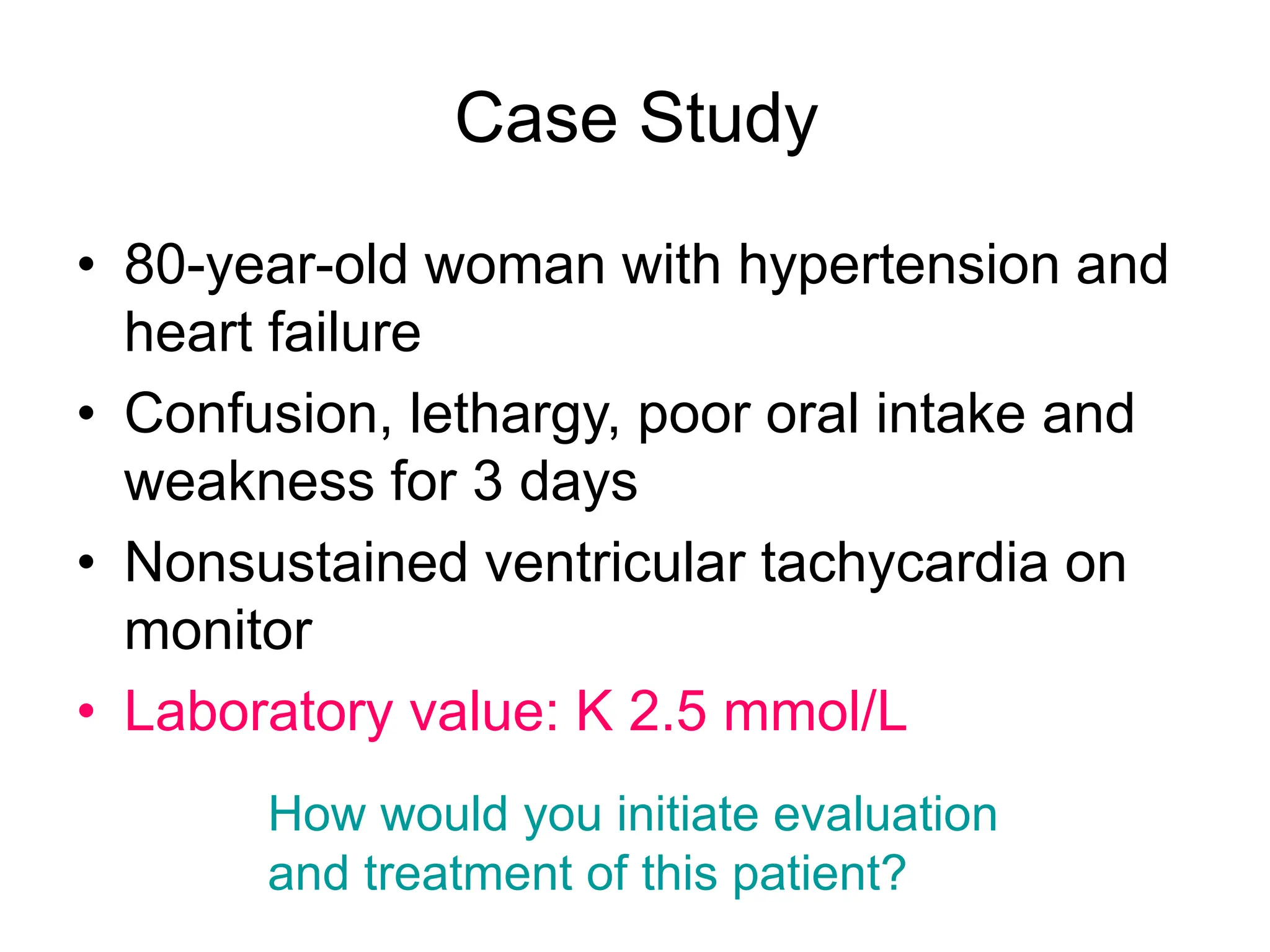
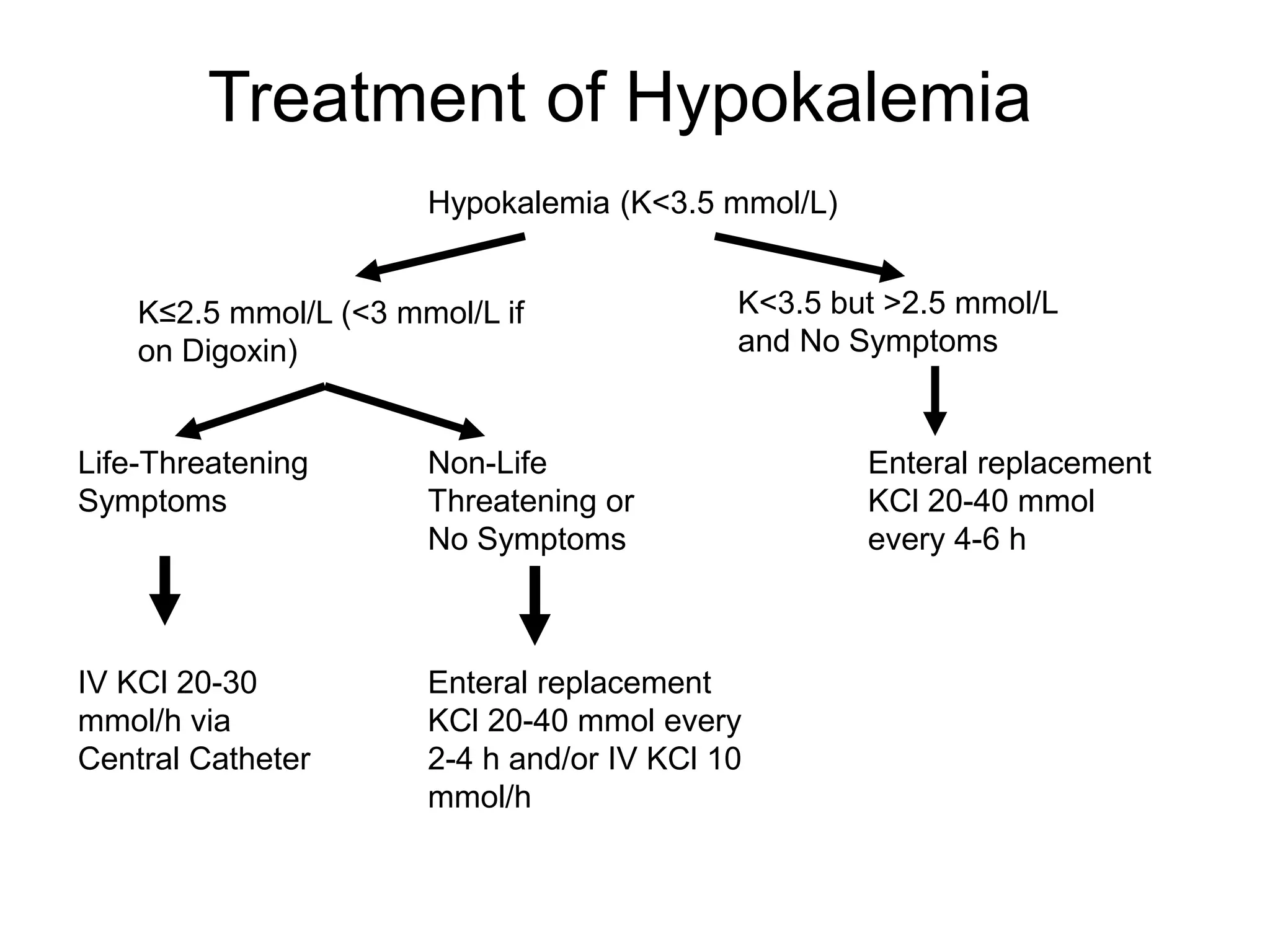
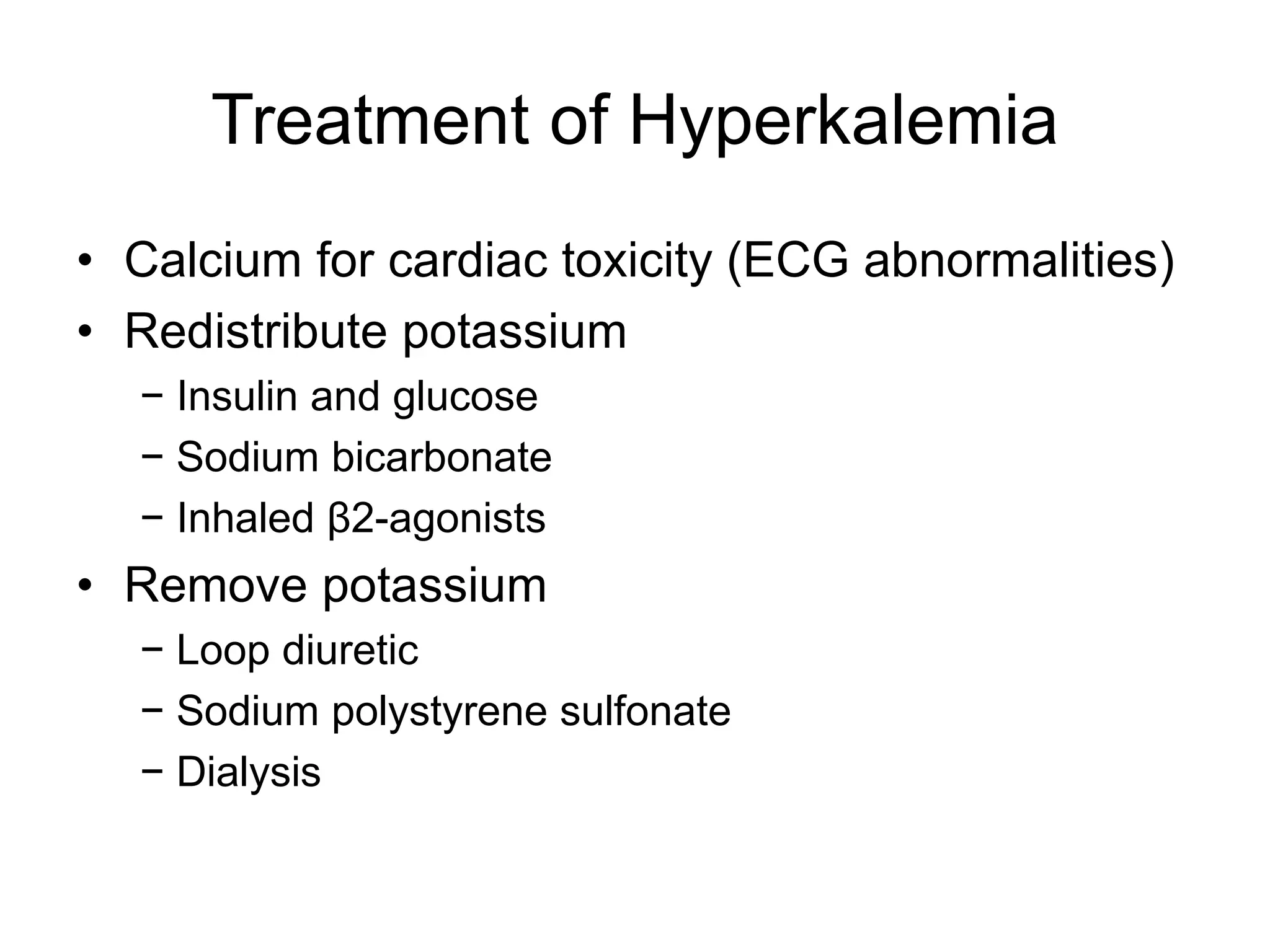
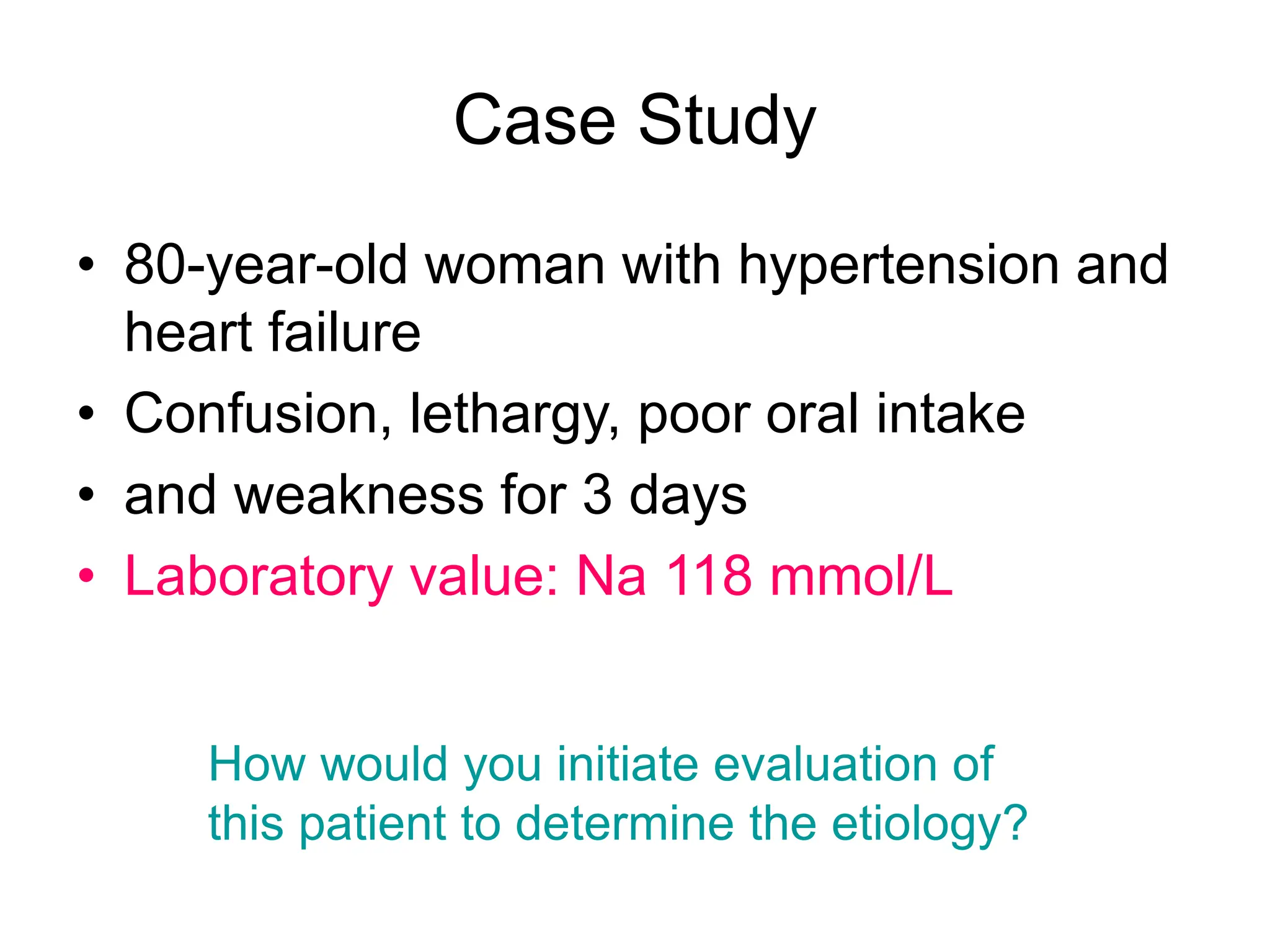
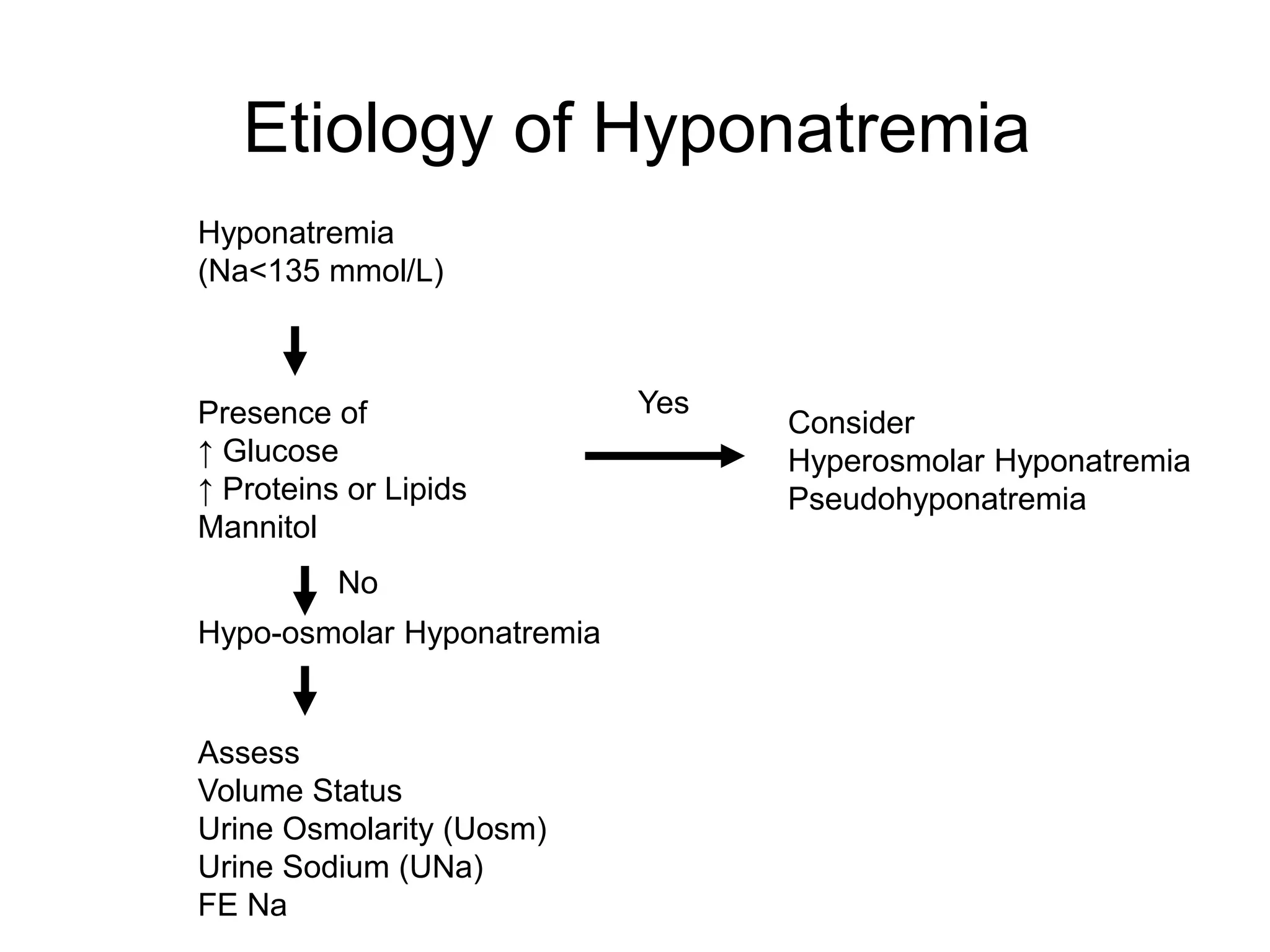
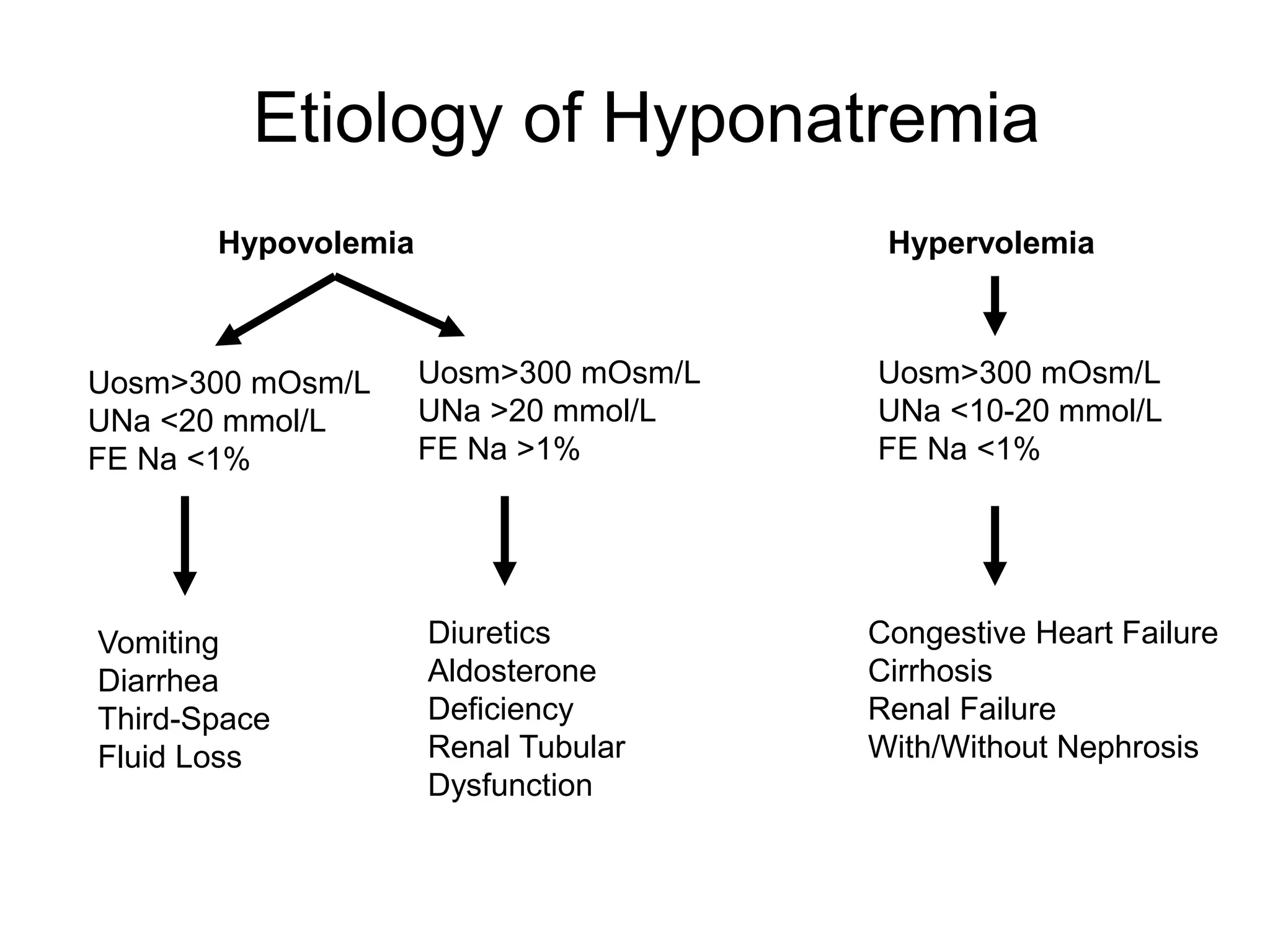
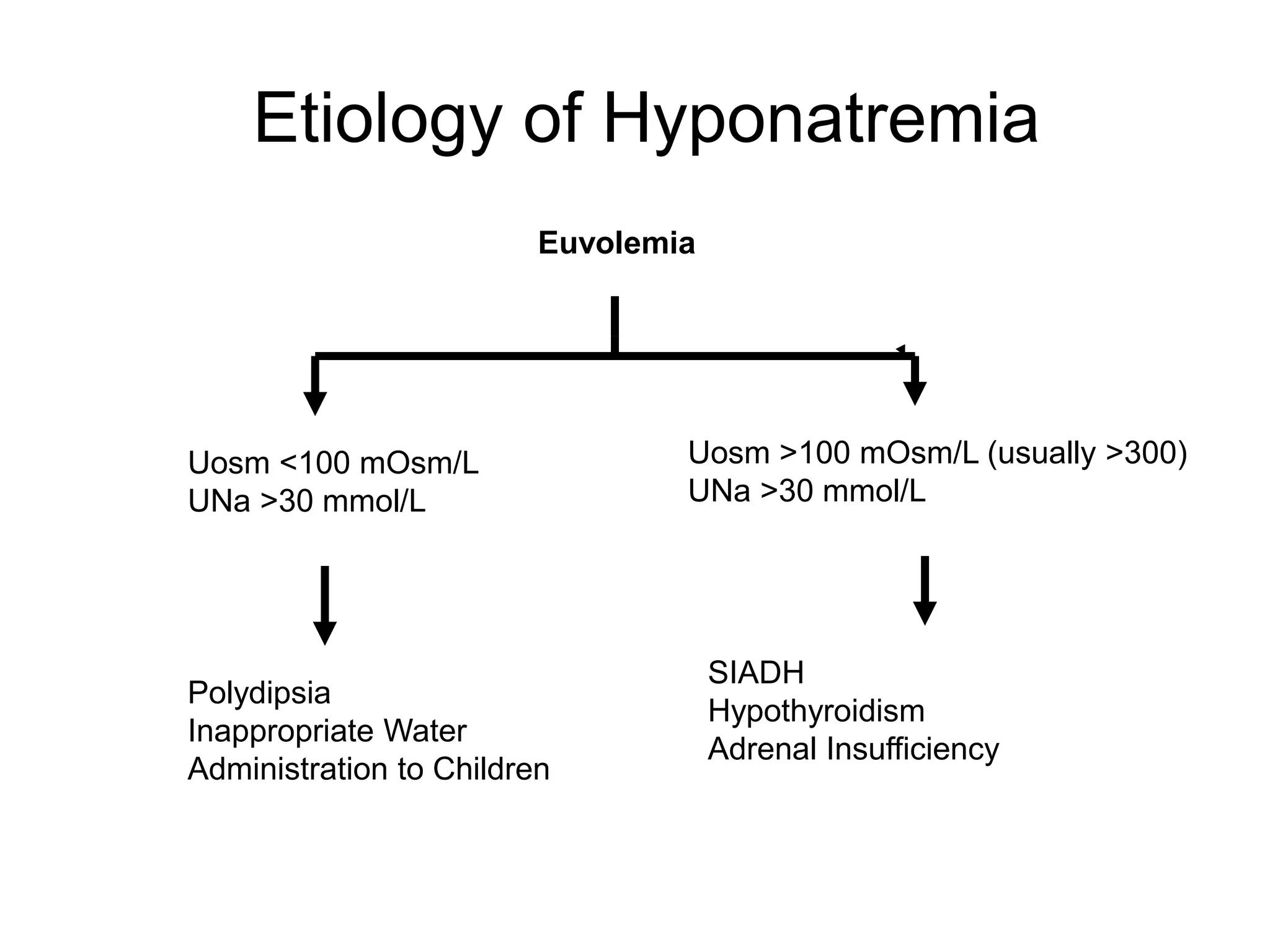
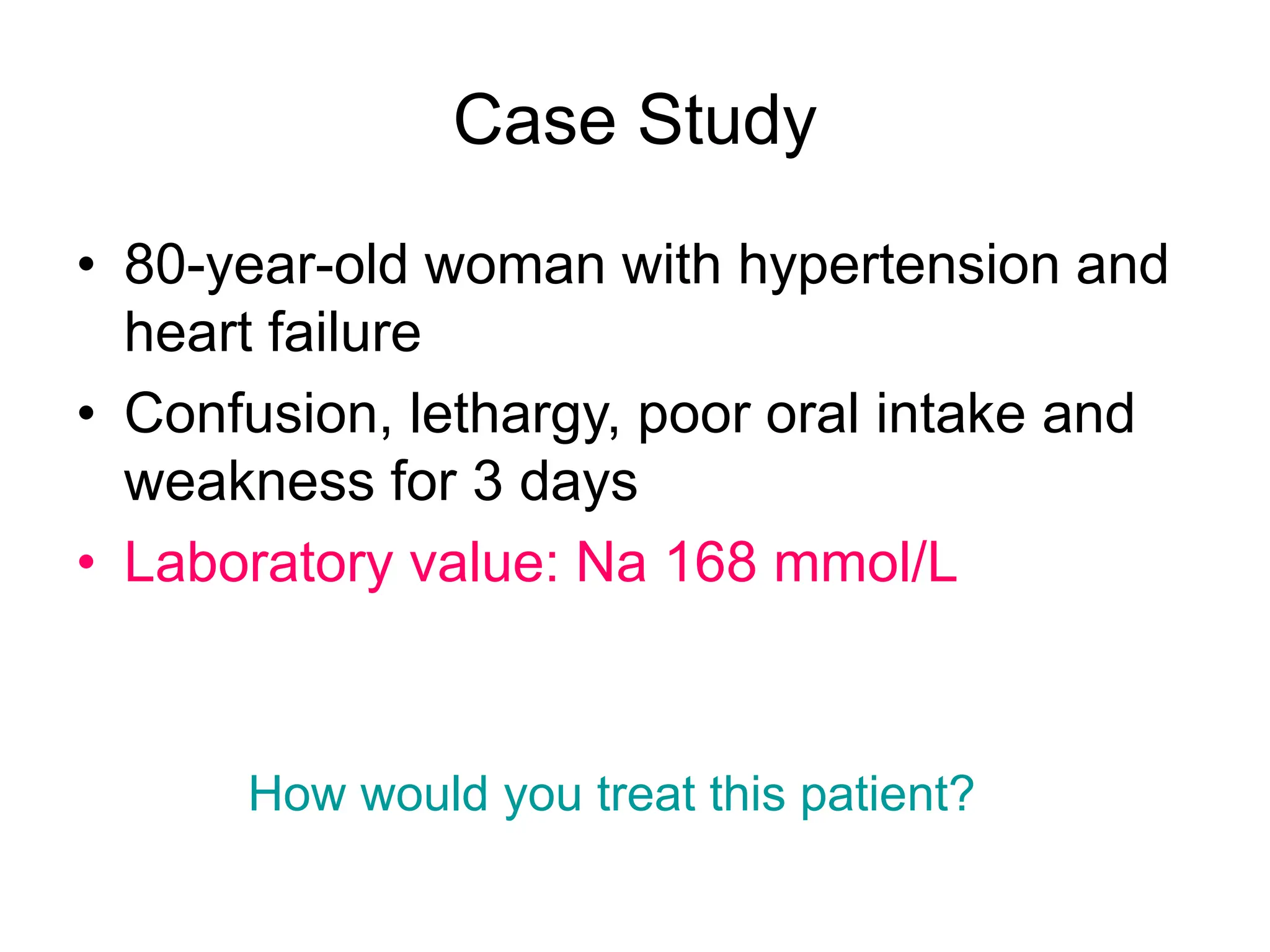
An 80-year-old woman presented with confusion, weakness, and nonsustained ventricular tachycardia. Her lab results showed hypokalemia (K=2.5 mmol/L), hyponatremia (Na=118 mmol/L), and she was started on IV potassium replacement. Further evaluation of her hyponatremia found she was euvolemic. Her sodium was then found to be elevated at 168 mmol/L and she received hypotonic fluids. Electrolyte imbalances can have serious consequences and require identifying the cause, urgent treatment if life-threatening, and monitoring for correction.
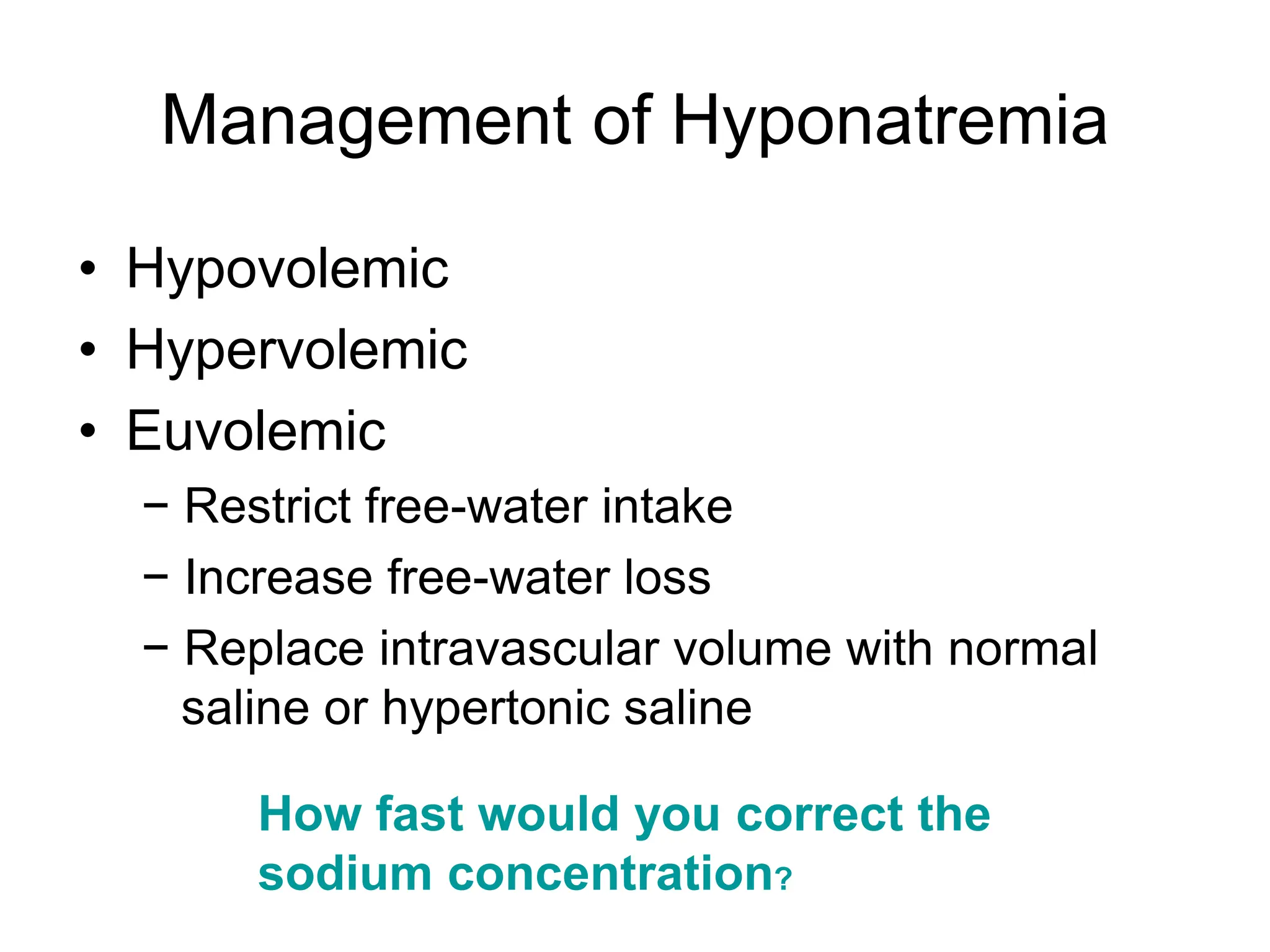
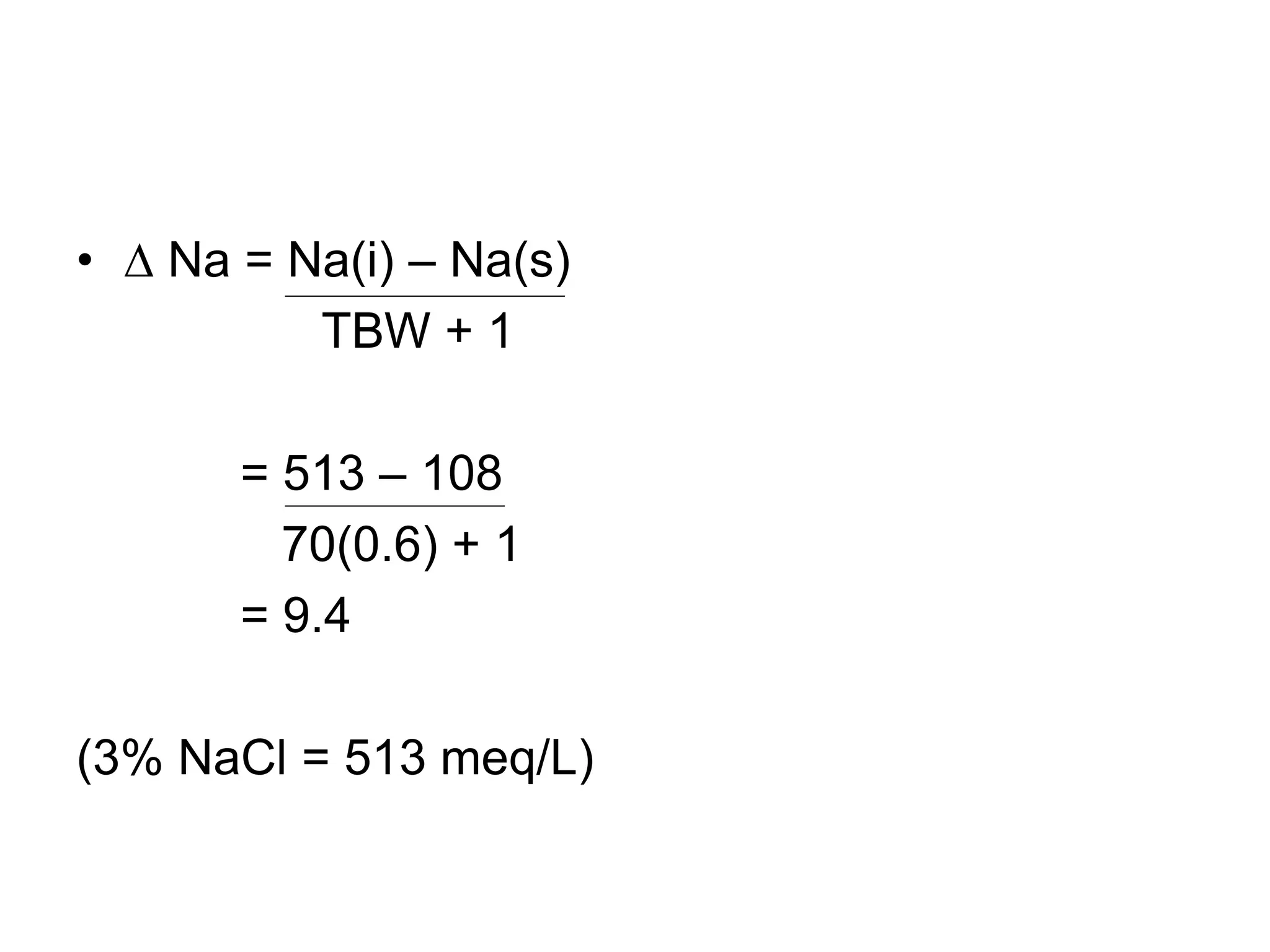
![Treatment of Hypernatremia
• Normal saline if hemodynamically unstable
• Hypotonic fluid when stable
− Intravenous fluids
− Enteral free water
• Quantity
H2O deficit (L) = [0.6 × wt (kg) ] × [Measured Na -140]
140
• Rate of correction](https://image.slidesharecdn.com/ccm01courseelectrolyteimbalance-240115190843-2f6806ab/75/CCM-01-Course-Electrolyte-Imbalance-ppt-15-2048.jpg)