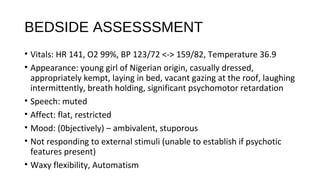
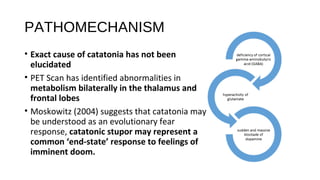
This document presents a case study of a 13-year old female patient who was admitted to hospital displaying symptoms of catatonia including psychomotor retardation, mutism, waxy flexibility, and staring episodes. The patient's symptoms and management are discussed in detail over her hospital stay. The document also provides background on catatonia as a historical concept, including its origins in the late 19th century and debates around its nosological status and relationship to other psychiatric conditions. Key figures who studied catatonia and helped develop understanding of the syndrome are also mentioned.