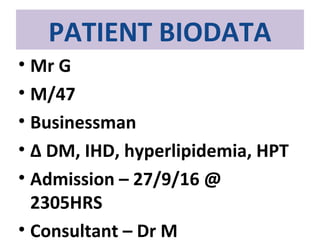
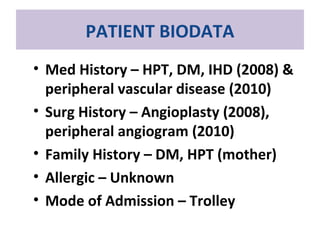
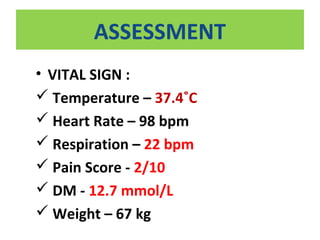
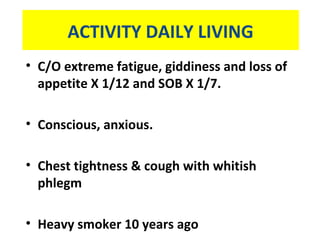
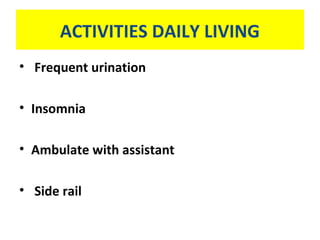
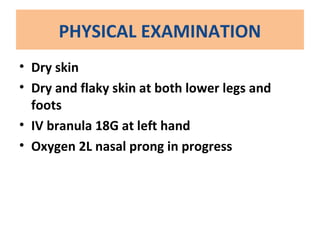
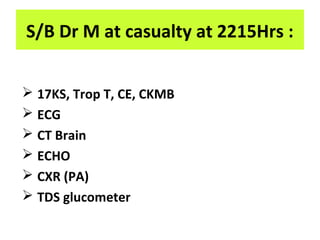
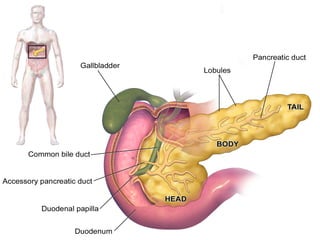
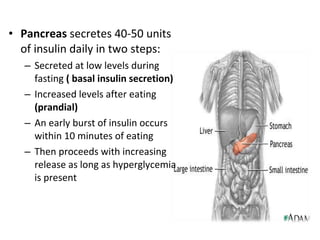
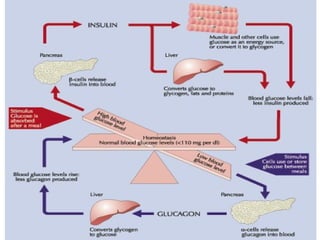
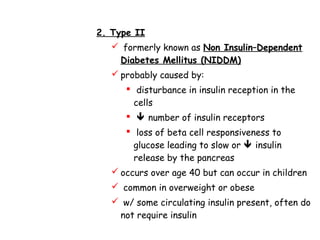
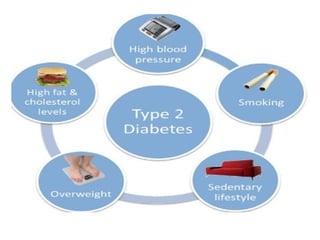
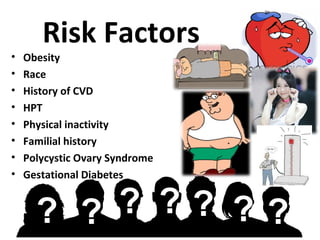
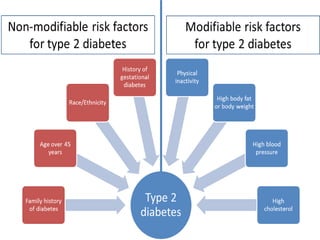
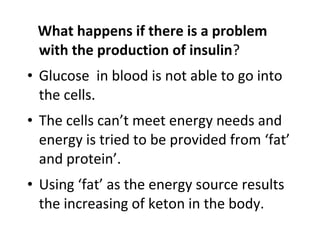
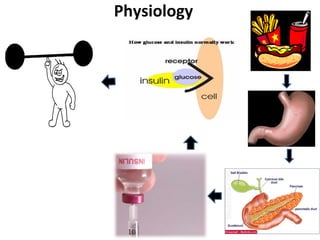
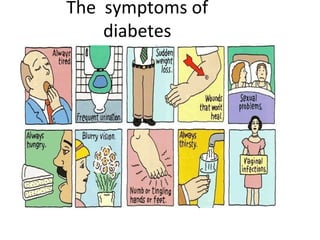
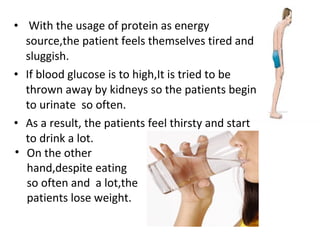
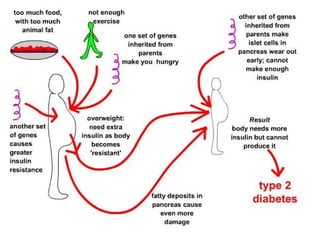
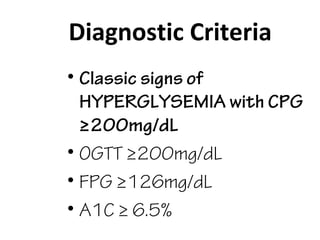
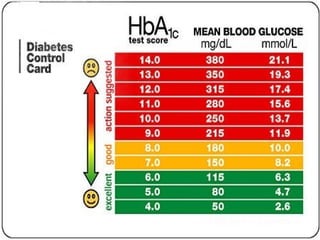
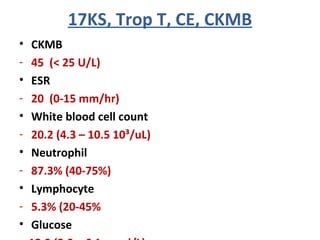
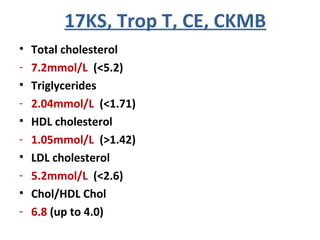
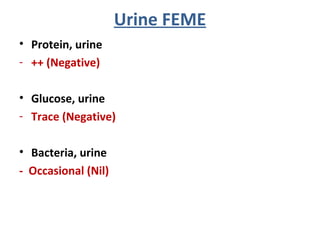
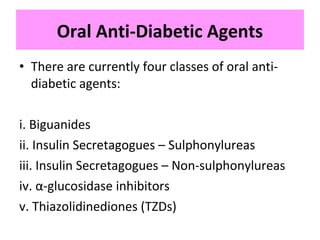
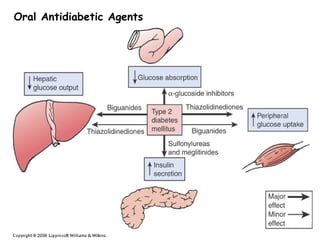
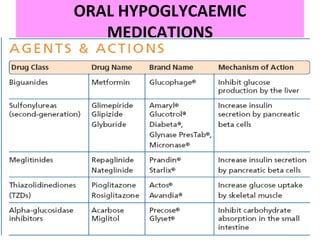
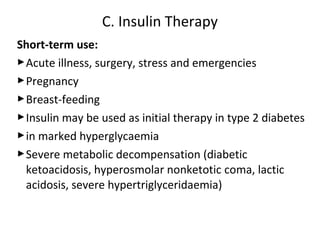
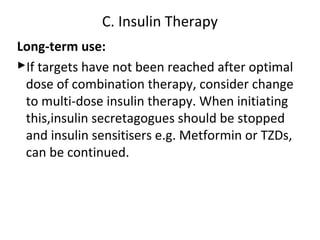
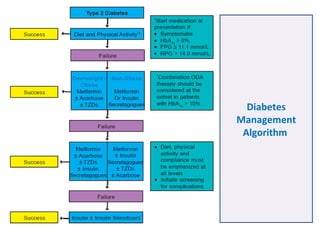
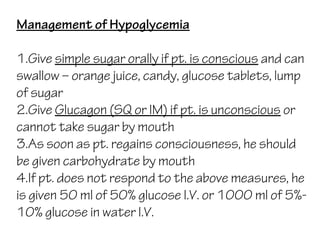
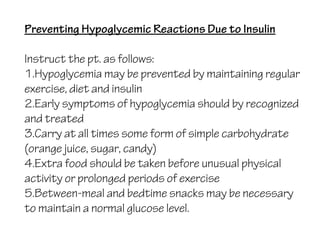
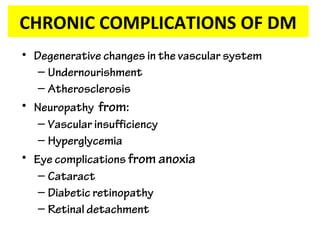
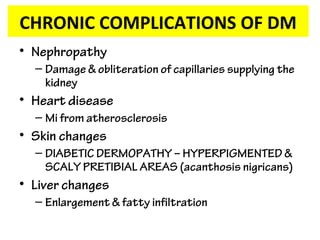
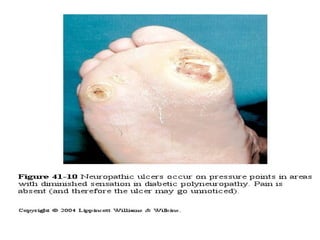
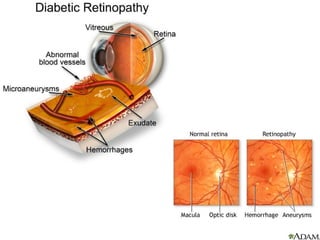
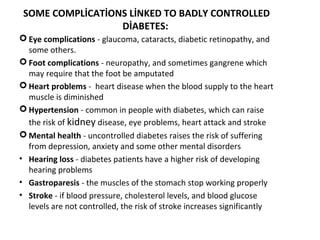
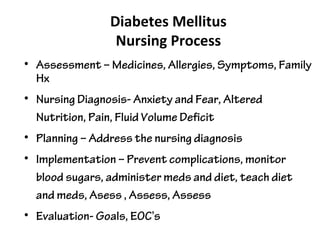
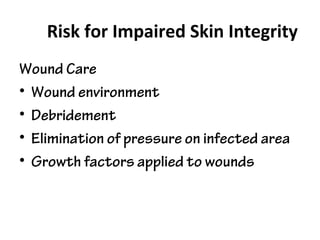
Mr. G, a 47-year-old businessman, was admitted to the hospital on September 27th at 11:05pm for diabetes mellitus, ischemic heart disease, hyperlipidemia, and hypertension. His medical history includes hypertension, diabetes, ischemic heart disease in 2008, and peripheral vascular disease in 2010. On examination, he had dry skin, flaky skin on his lower legs and feet, and an IV in his left hand. Lab tests showed elevated glucose, cholesterol, and kidney function. Imaging found an old heart attack and brain infarct. The patient's diabetes is managed through diet, exercise, oral medications, and possibly insulin therapy depending on his ability to control blood sugar levels.