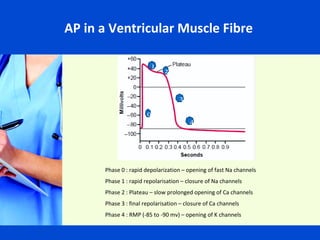
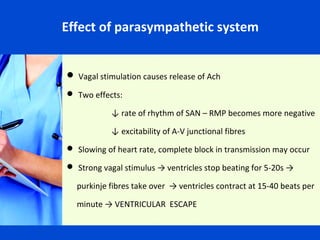
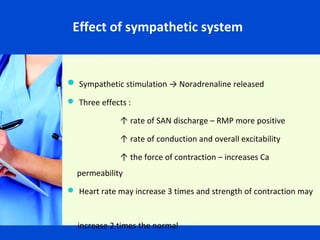
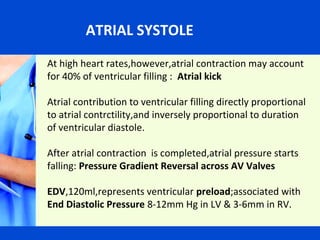
The document summarizes the cardiac cycle, including the electrical and mechanical events of the heart. It describes the conduction system that controls heart rhythm, including the sinoatrial node as the pacemaker. The main phases of the cardiac cycle are described in detail: atrial systole, isovolumetric contraction, ejection, isovolumetric relaxation, and ventricular filling. Pressure values for the different chambers are also provided. The coordination of these electrical and mechanical events ensures effective pumping of blood throughout the cardiovascular system.