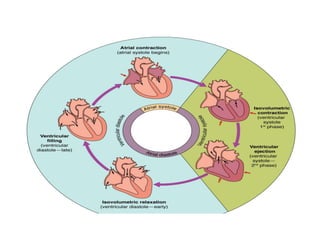
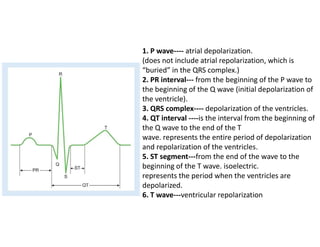
The document discusses the phases of the cardiac cycle and relates electrocardiogram readings, pressure changes in the atria and ventricles, volume changes in the ventricles, and heart sounds to each phase. It describes the seven phases: 1) atrial systole, 2) isovolumetric ventricular contraction, 3) rapid ventricular ejection, 4) reduced ventricular ejection, 5) isovolumetric ventricular relaxation, 6) rapid ventricular filling, and 7) reduced ventricular filling. Key details covered include the relationship between phases and P waves, QRS complex, T waves, and the four heart sounds.