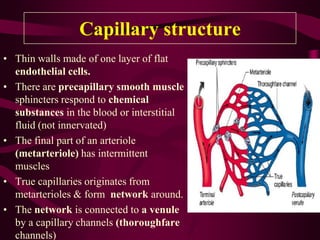
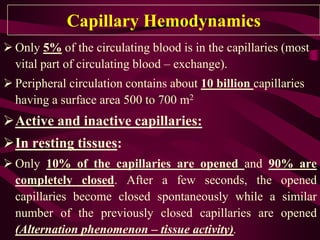
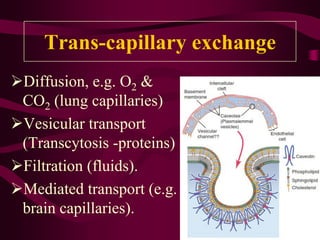
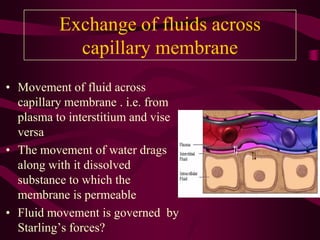
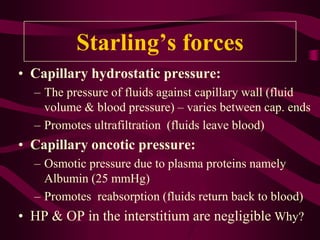
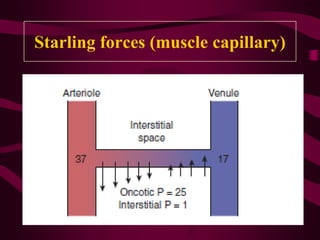
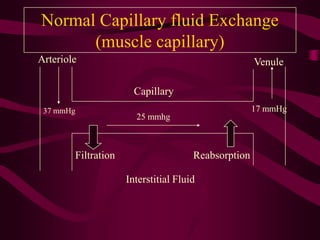
This document discusses capillary circulation and trans-capillary exchange. It begins by outlining the objectives and structure of capillaries, including their thin endothelial walls, precapillary sphincters, and connections to arterioles and venules. It then explains capillary functions like nutrient/oxygen exchange, waste drainage, and temperature regulation. Trans-capillary exchange via diffusion, vesicular transport, and filtration is also summarized. Starling's forces that govern fluid movement across capillary membranes are defined. Finally, the document discusses edema, including its definition and causes like increased hydrostatic pressure, decreased oncotic pressure, lymphatic obstruction, and increased permeability.