This document discusses calcium homeostasis, including the physiological importance of calcium, its distribution and forms in the body, and how blood calcium levels are regulated. The key points are:
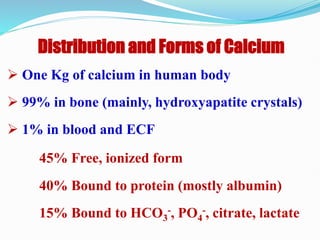
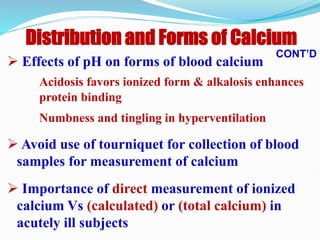
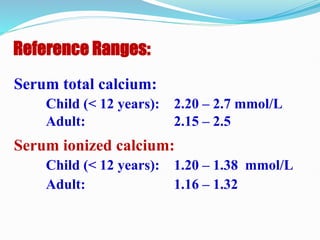
1) Calcium is important for neuromuscular excitability, blood coagulation, bone mineralization, and hormone/neurotransmitter release. 99% is stored in bones, while 1% is in blood/extracellular fluid.
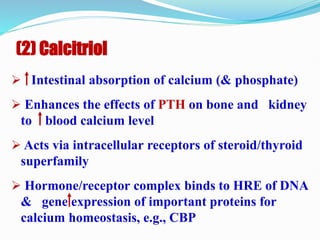
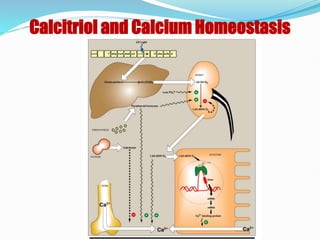
2) Blood calcium levels are regulated by parathyroid hormone (PTH), calcitriol (the active form of vitamin D), and calcitonin. PTH and calcitriol work to increase blood calcium by acting on bones, kidneys, and intestines.