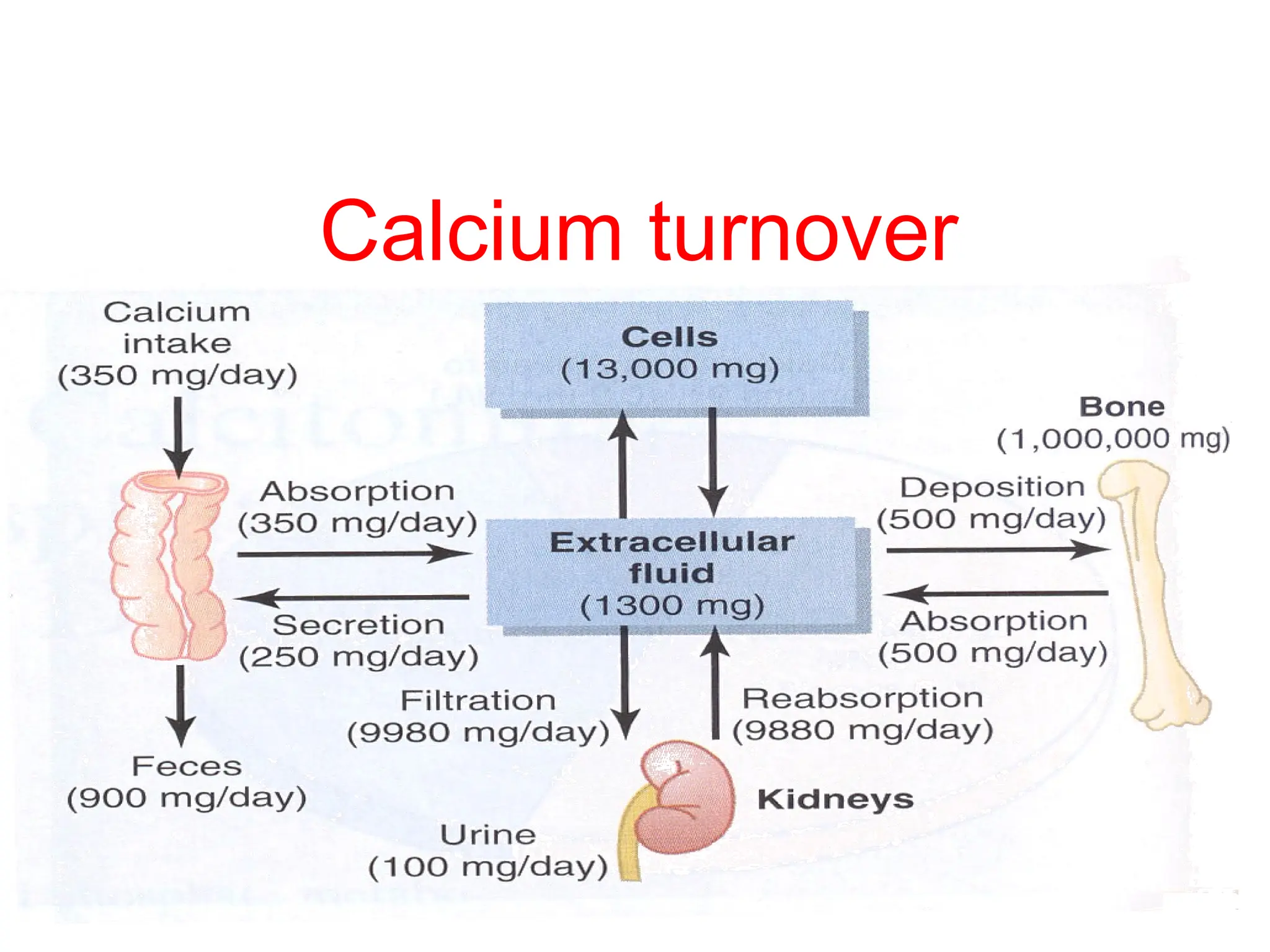
The document provides detailed information on calcium metabolism, including its distribution in the body, dietary requirements by age, absorption mechanisms, and the biological functions of calcium. It discusses the regulatory hormones such as parathyroid hormone (PTH) and calcitonin, explaining their roles in maintaining calcium homeostasis, as well as the synthesis and action of vitamin D3. Additionally, it covers the physiological implications of calcium levels on bone metabolism and overall health.















![Regulation of PTH
The dominant regulator of PTH is plasma Ca2+
.
Secretion of PTH is inversely related to [Ca2+
].
Maximum secretion of PTH occurs at plasma Ca2+
below 3.5 mg/dL.
At Ca2+
above 5.5 mg/dL, PTH secretion is maximally inhibited.
PTH secretion responds to small alterations in plasma Ca2+
within
seconds
A unique calcium receptor within the parathyroid cell plasma membrane
senses changes in the extracellular fluid concentration of Ca2+
.](https://image.slidesharecdn.com/calciummetabolism-240814080938-c341fe05/75/calcium-metabolism-pptx-17-2048.jpg)




