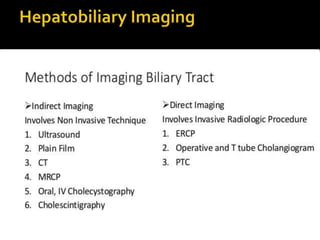
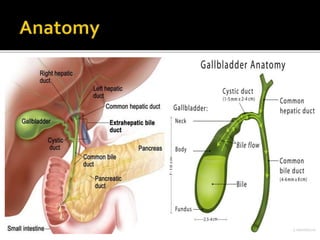
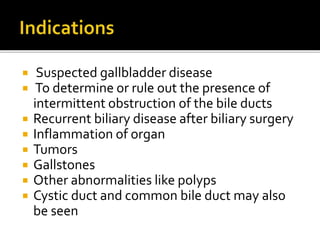
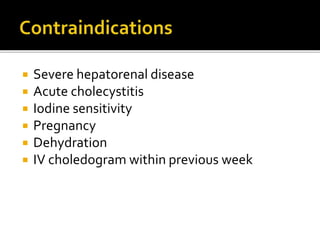
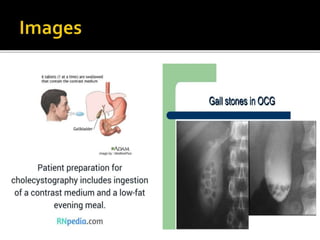
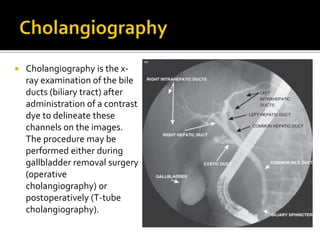
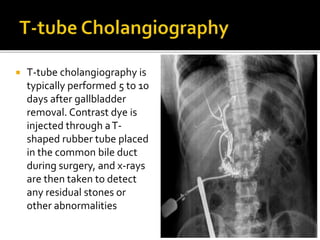
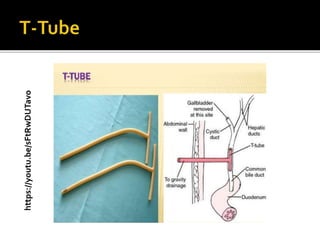
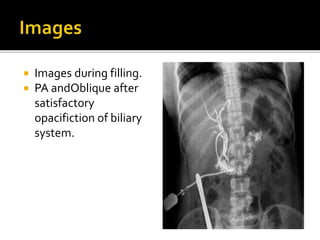
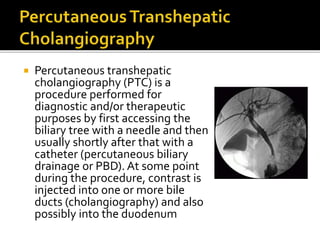
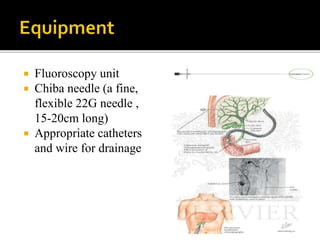
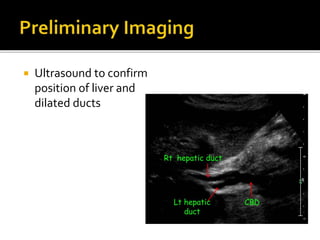
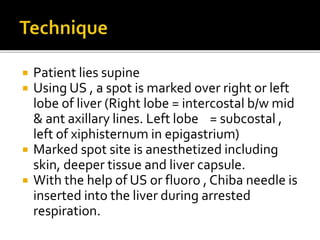
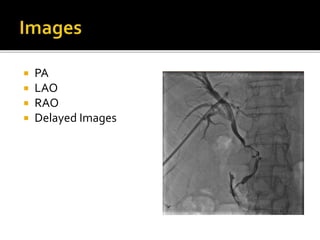
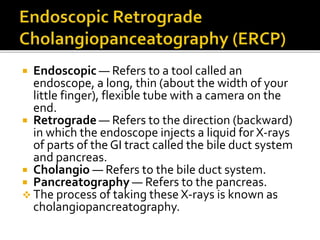
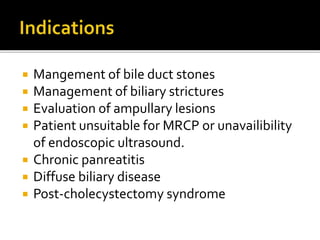
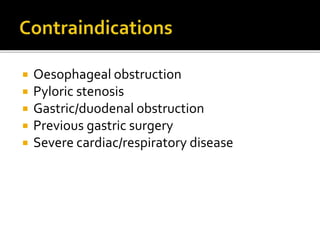
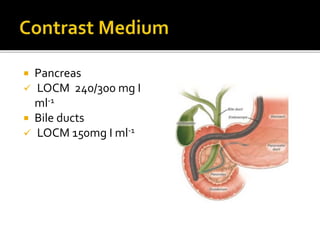
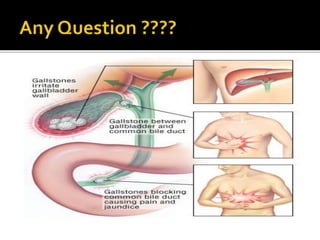
The document discusses various radiographic procedures used to examine the gallbladder and biliary tract, including oral cholecystography, cholangiography, T-tube cholangiography, and ERCP (endoscopic retrograde cholangiopancreatography). It provides details on the indications, contraindications, procedures, and imaging for each type of examination. The various procedures are used to visualize the gallbladder and bile ducts, detect gallstones or other abnormalities, and manage biliary diseases.