- Bronchiectasis refers to irreversible dilation of the airways and can be focal or diffuse. It has various causes including infection, immunodeficiency, genetic conditions, and autoimmune diseases.
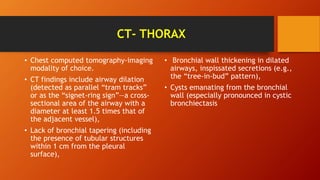
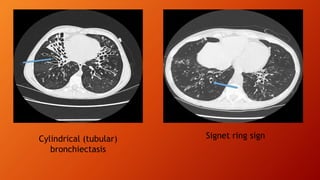
- Patients present with a persistent productive cough and thick sputum. Diagnosis is made through chest imaging like CT scan which shows dilated and thick-walled airways.
- Treatment involves controlling infections with antibiotics, improving secretion clearance with airway clearance techniques, and minimizing further infection risk with long-term preventative strategies like daily or rotating oral antibiotics.