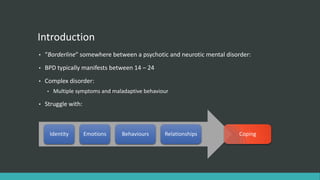
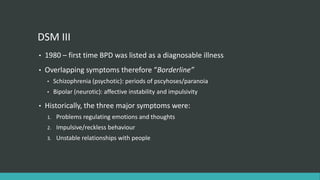
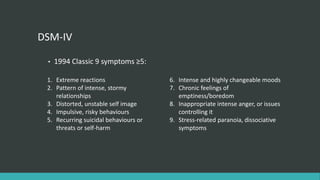
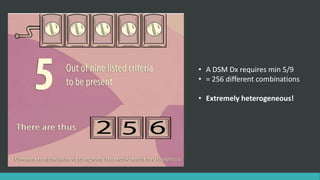
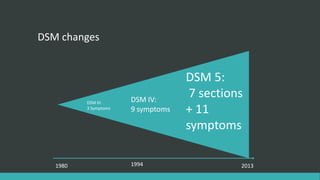
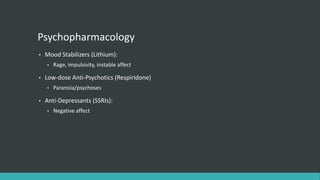
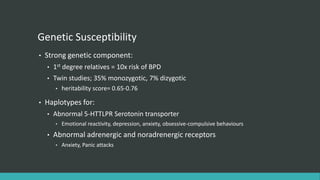
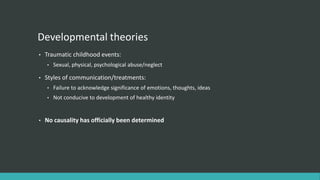
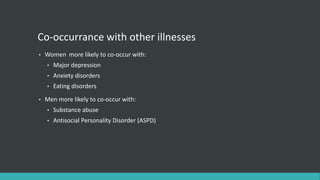
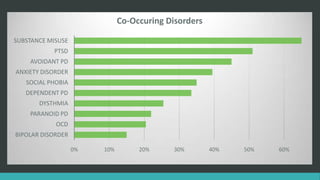
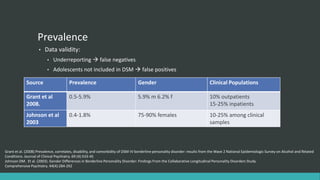
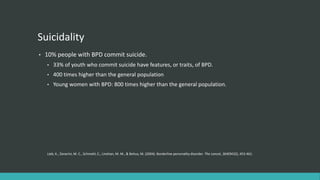
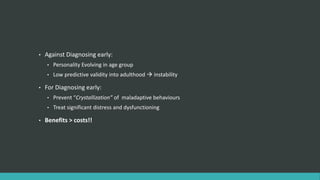
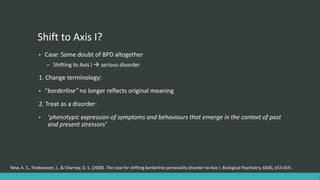
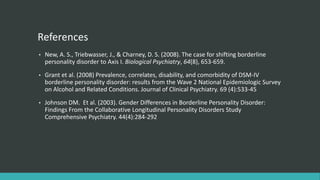
Borderline Personality Disorder (BPD) is a complex mental disorder characterized by difficulties regulating emotions and impulsive behaviors. It typically emerges during late adolescence/early adulthood. While treatments like DBT and medication can help manage symptoms, BPD has high rates of suicide and comorbidity with other disorders. The causes are debated but may involve genetic and environmental factors like childhood trauma. BPD prevalence is estimated around 1-6% but is more common in clinical populations. It can cause significant impairment so early diagnosis and prevention are important.