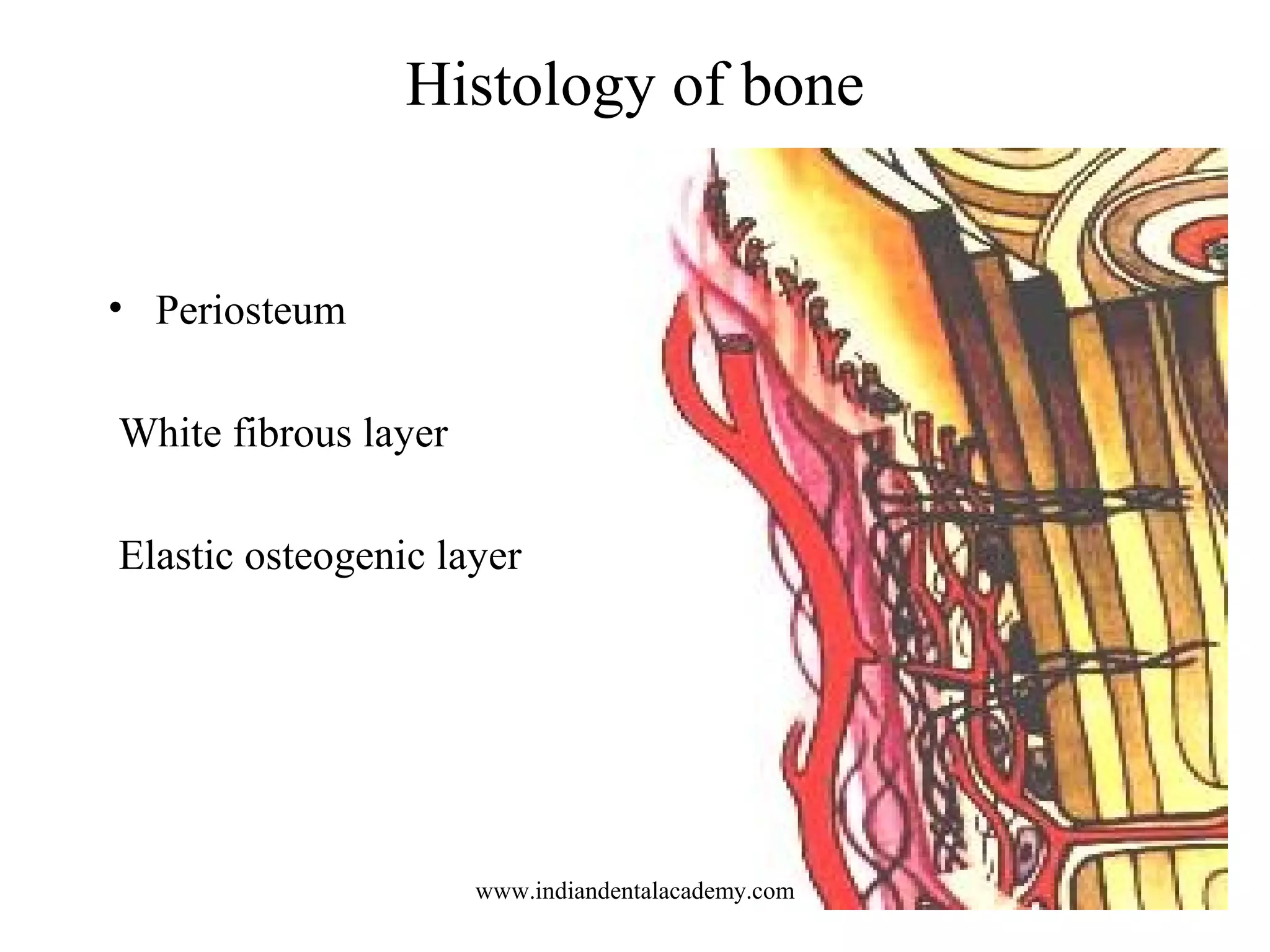
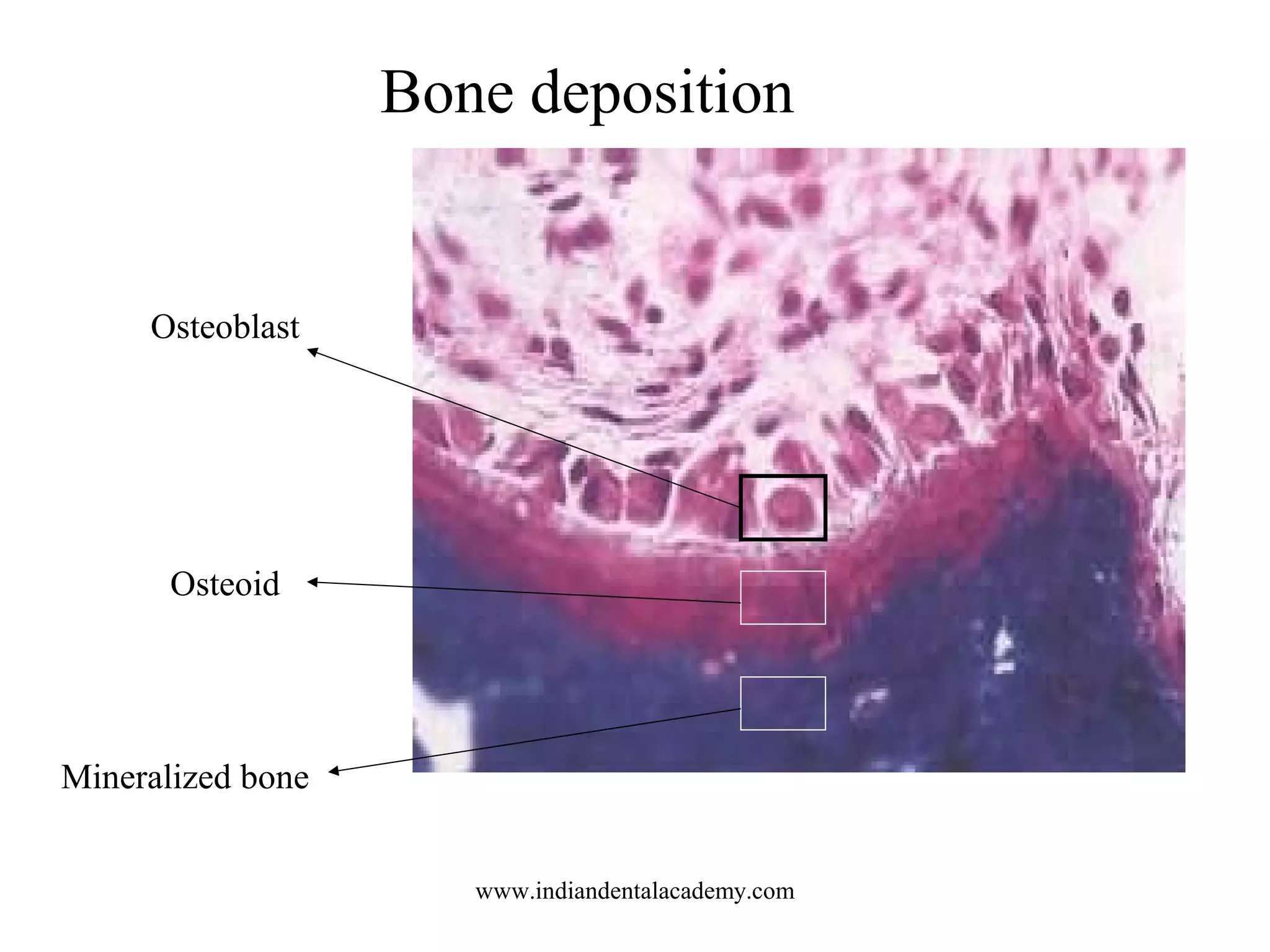
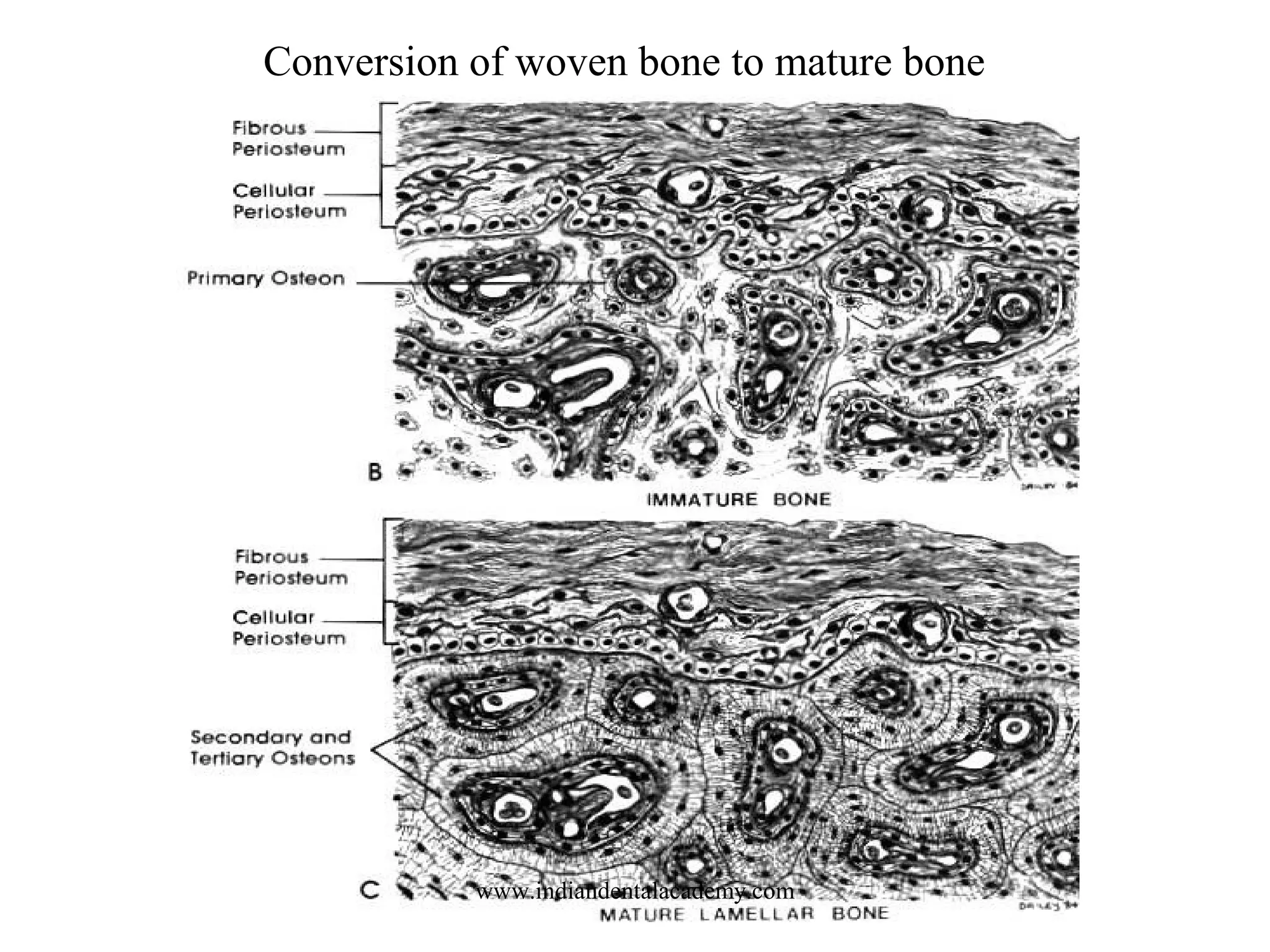
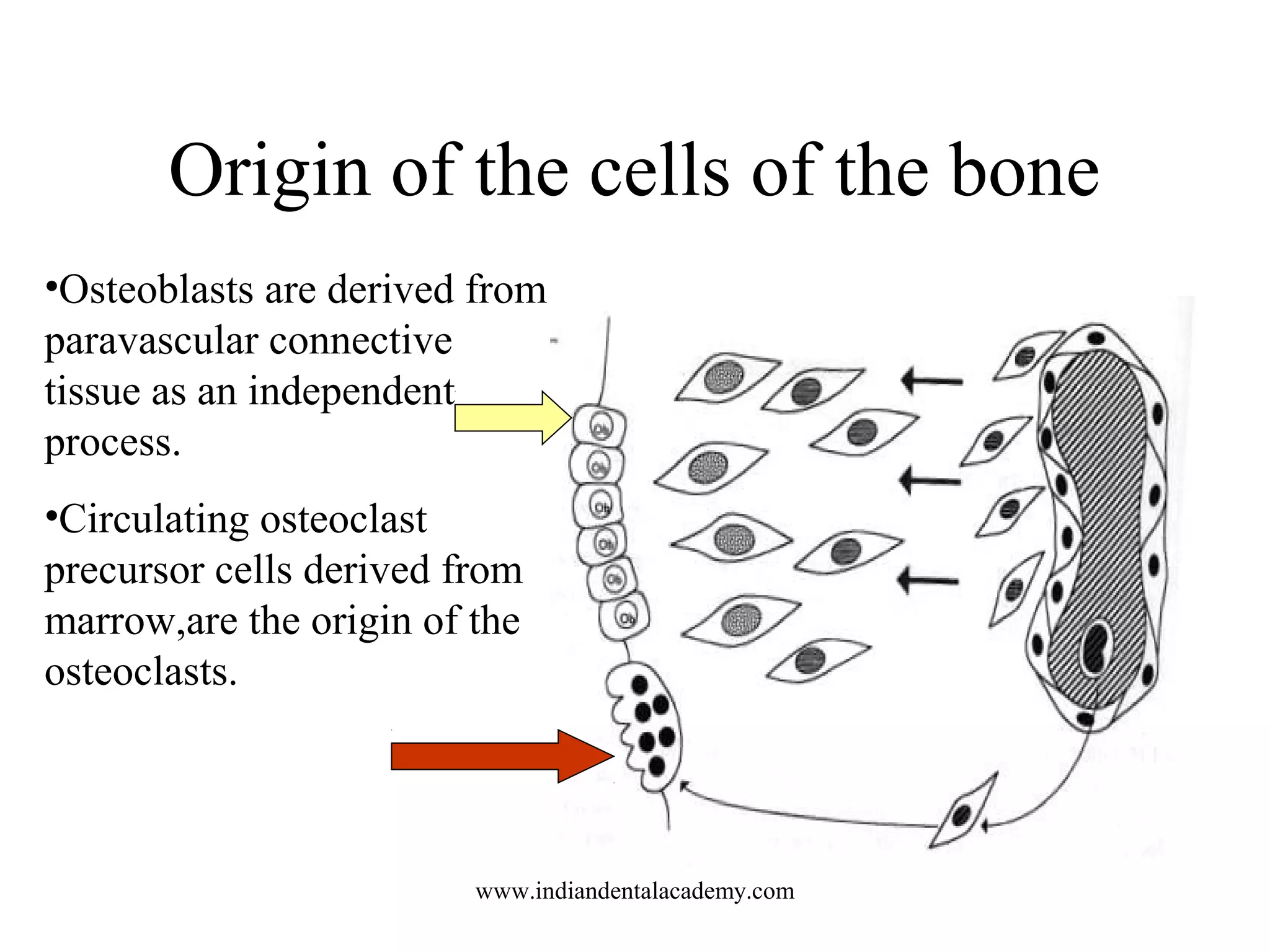
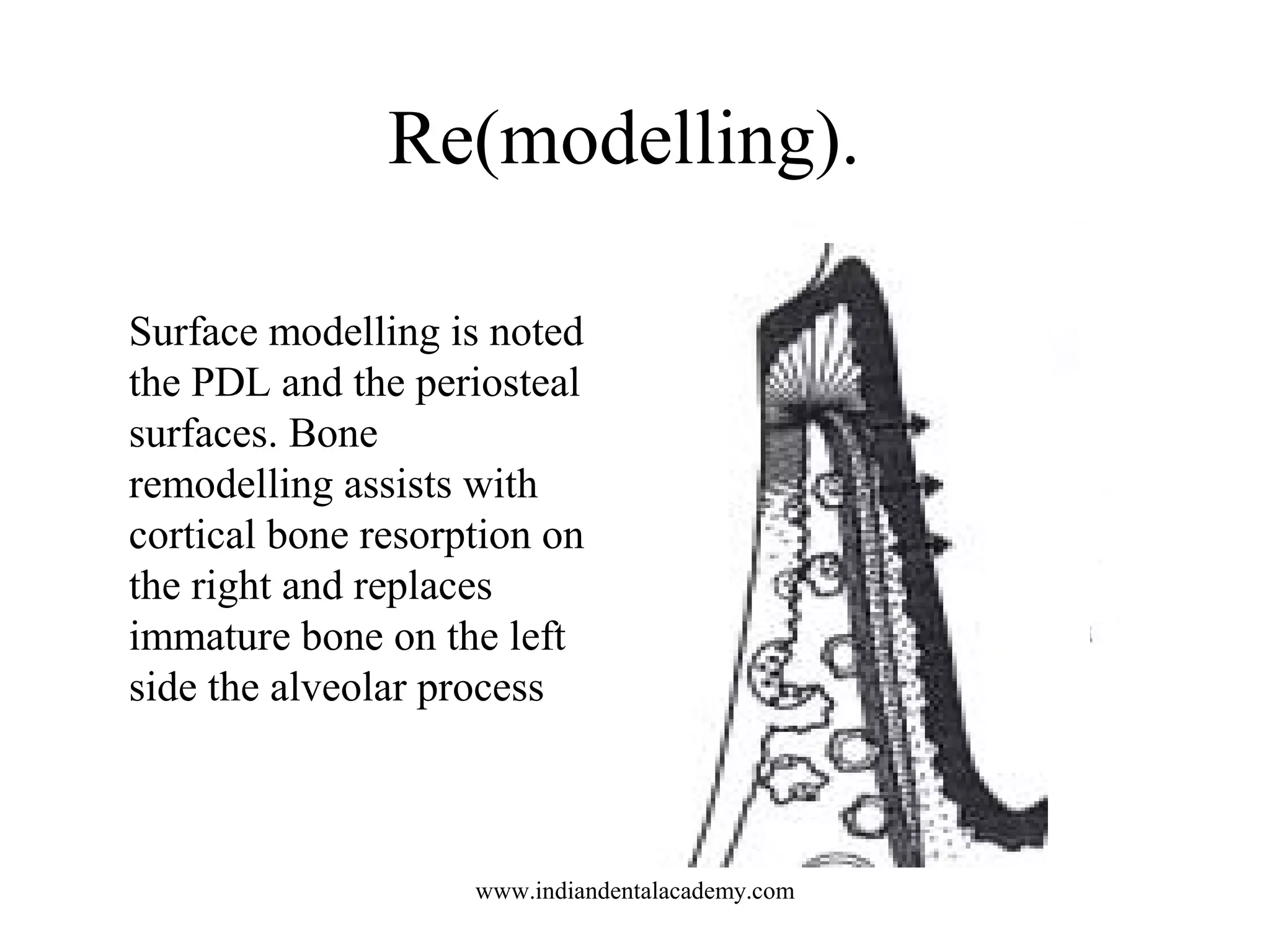
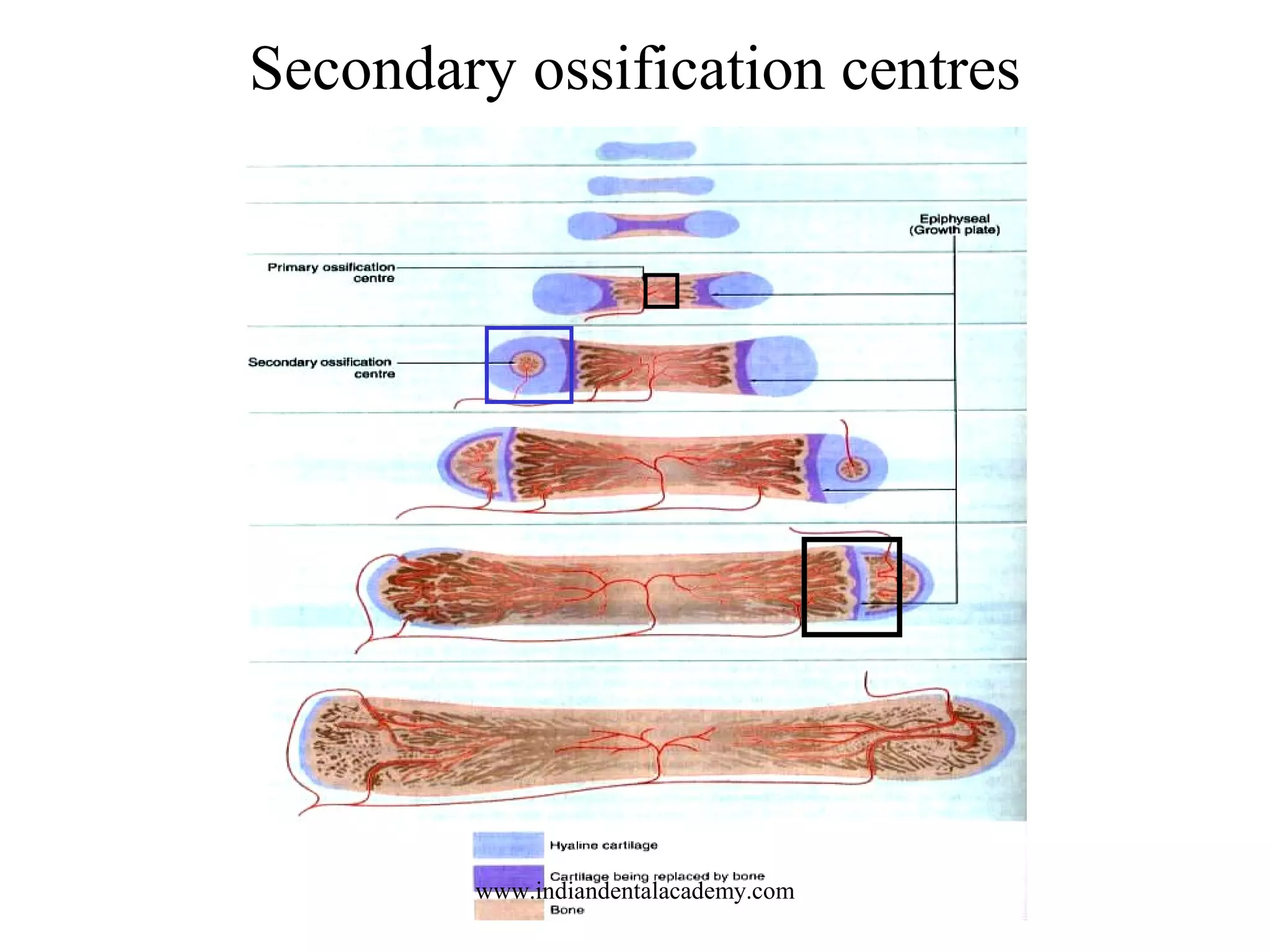
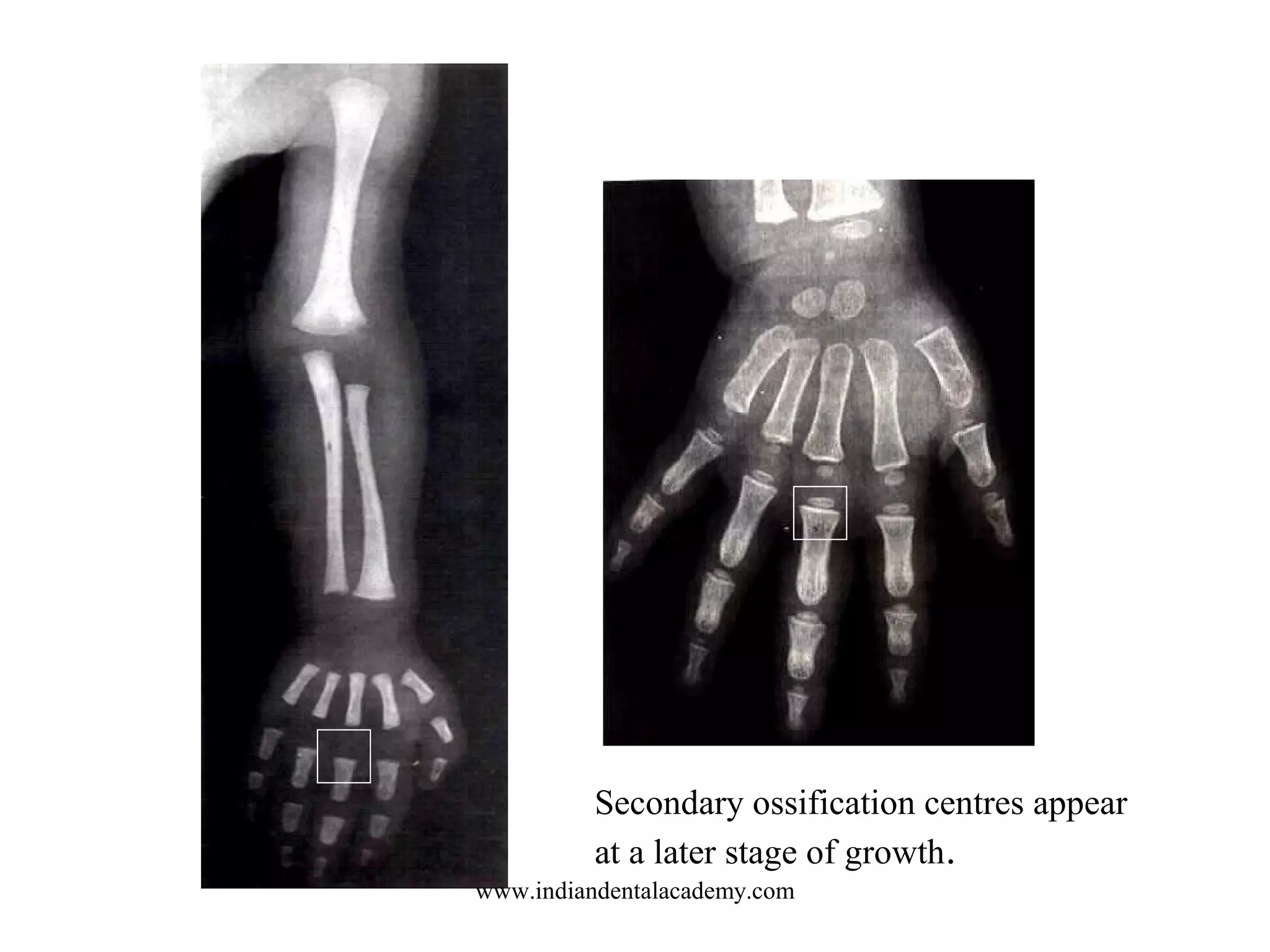
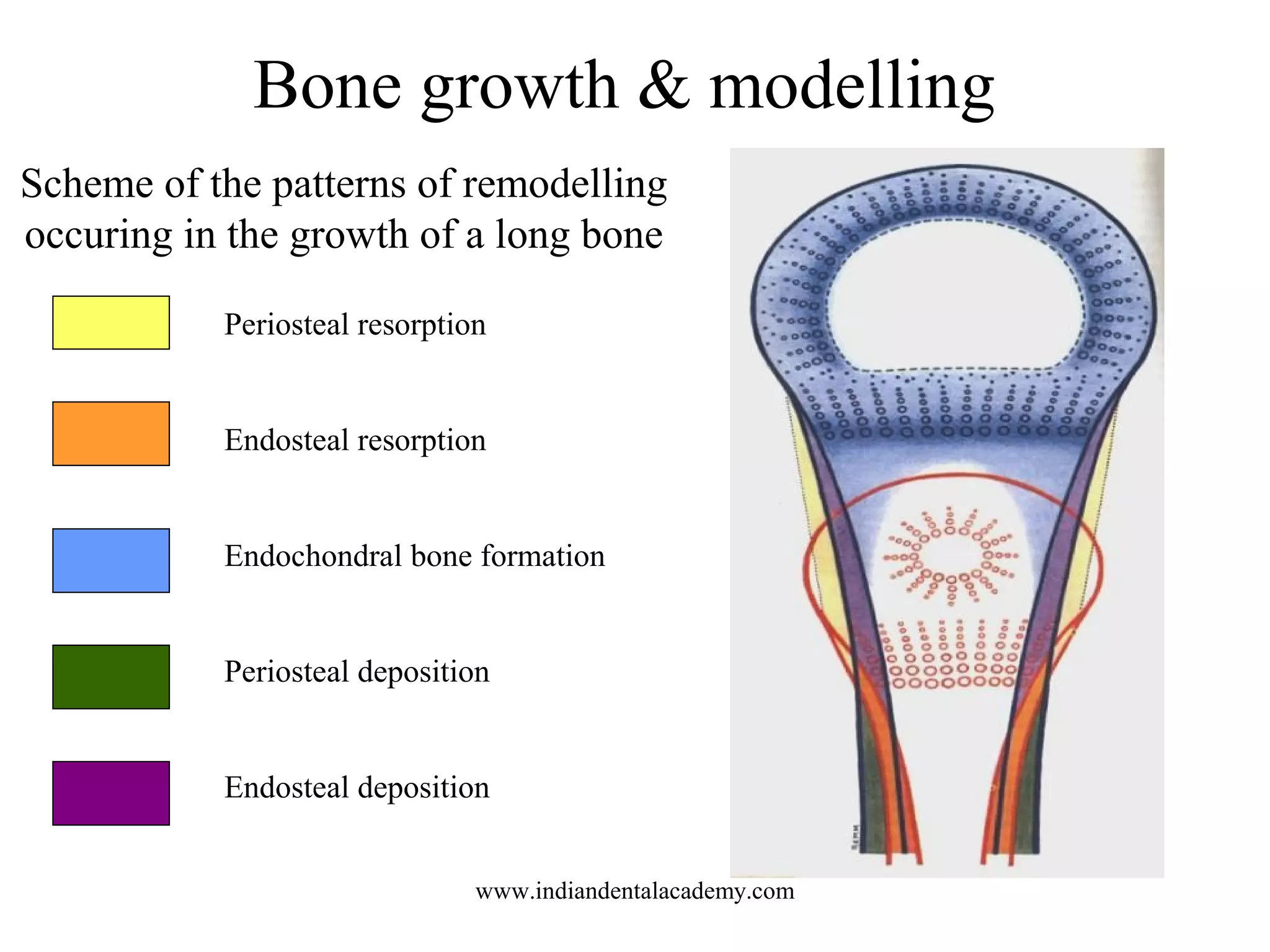
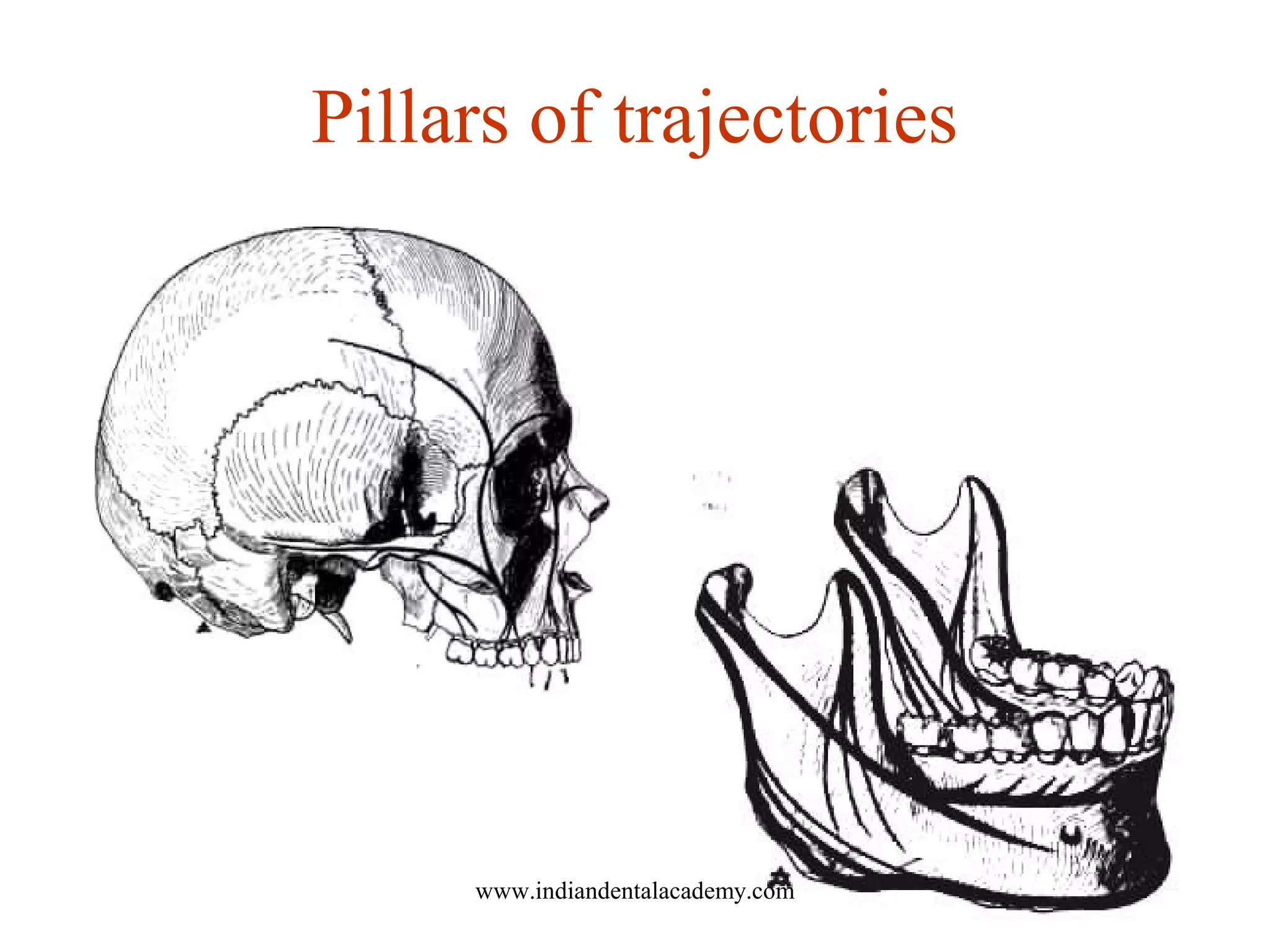
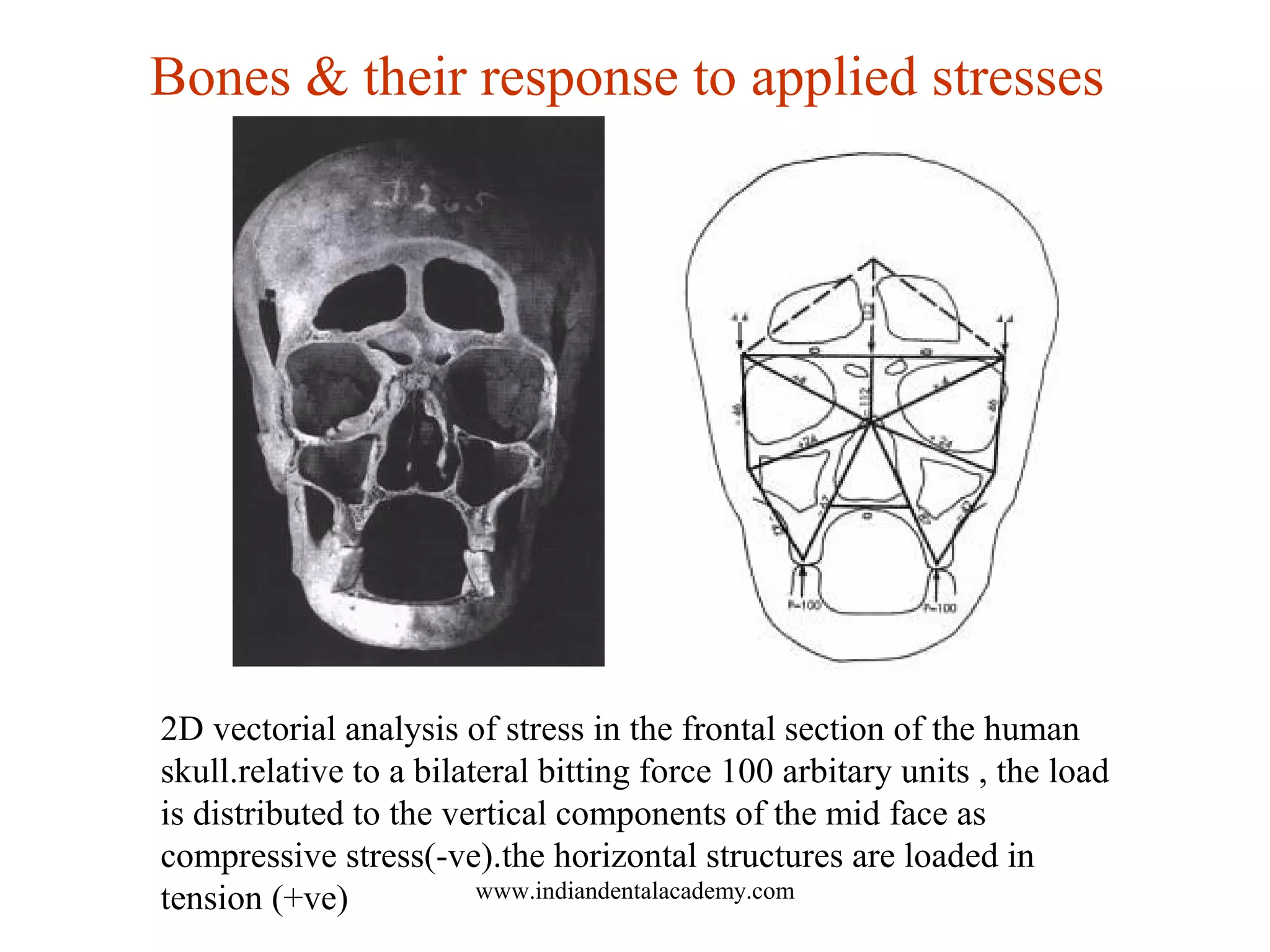
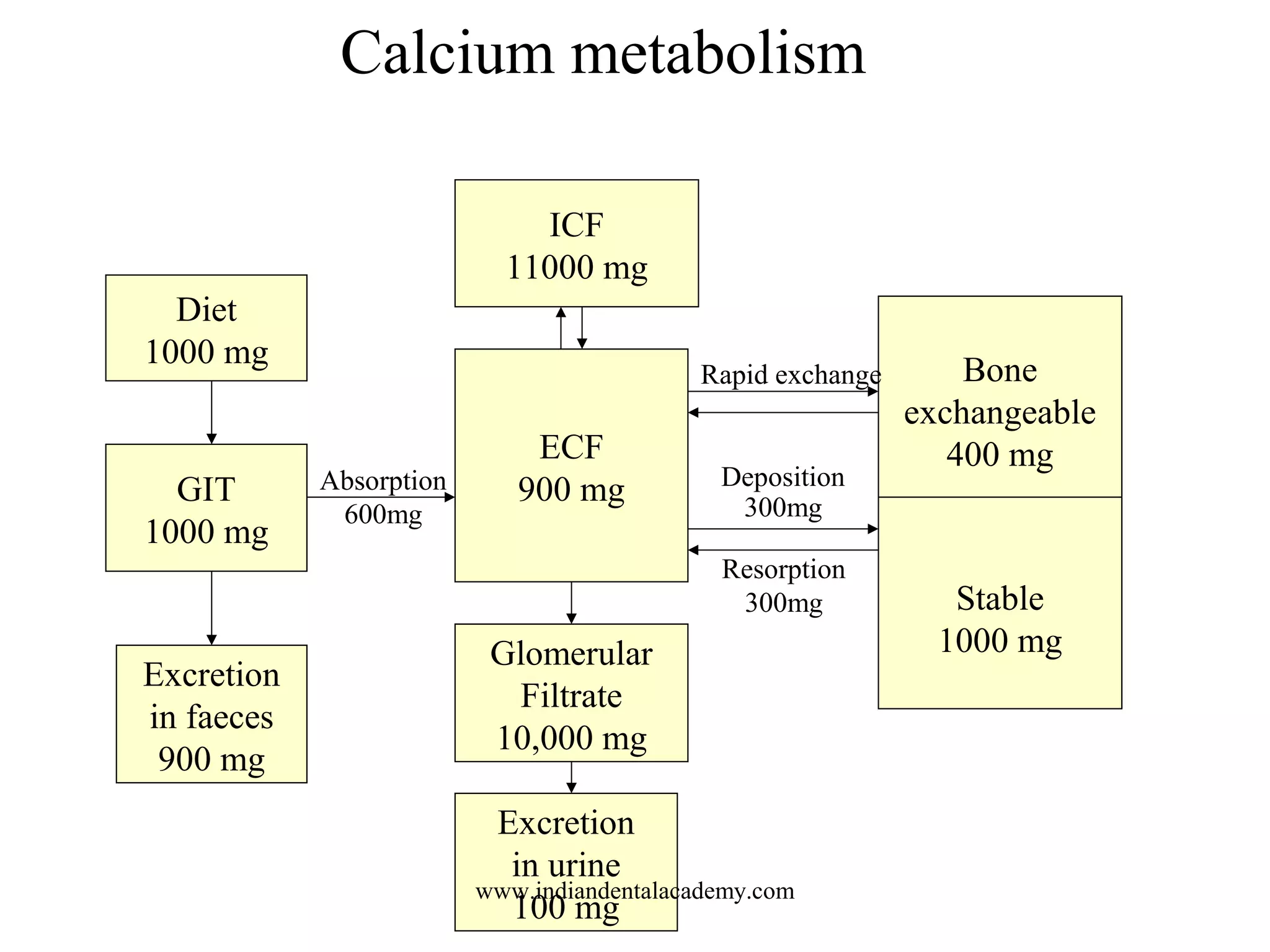
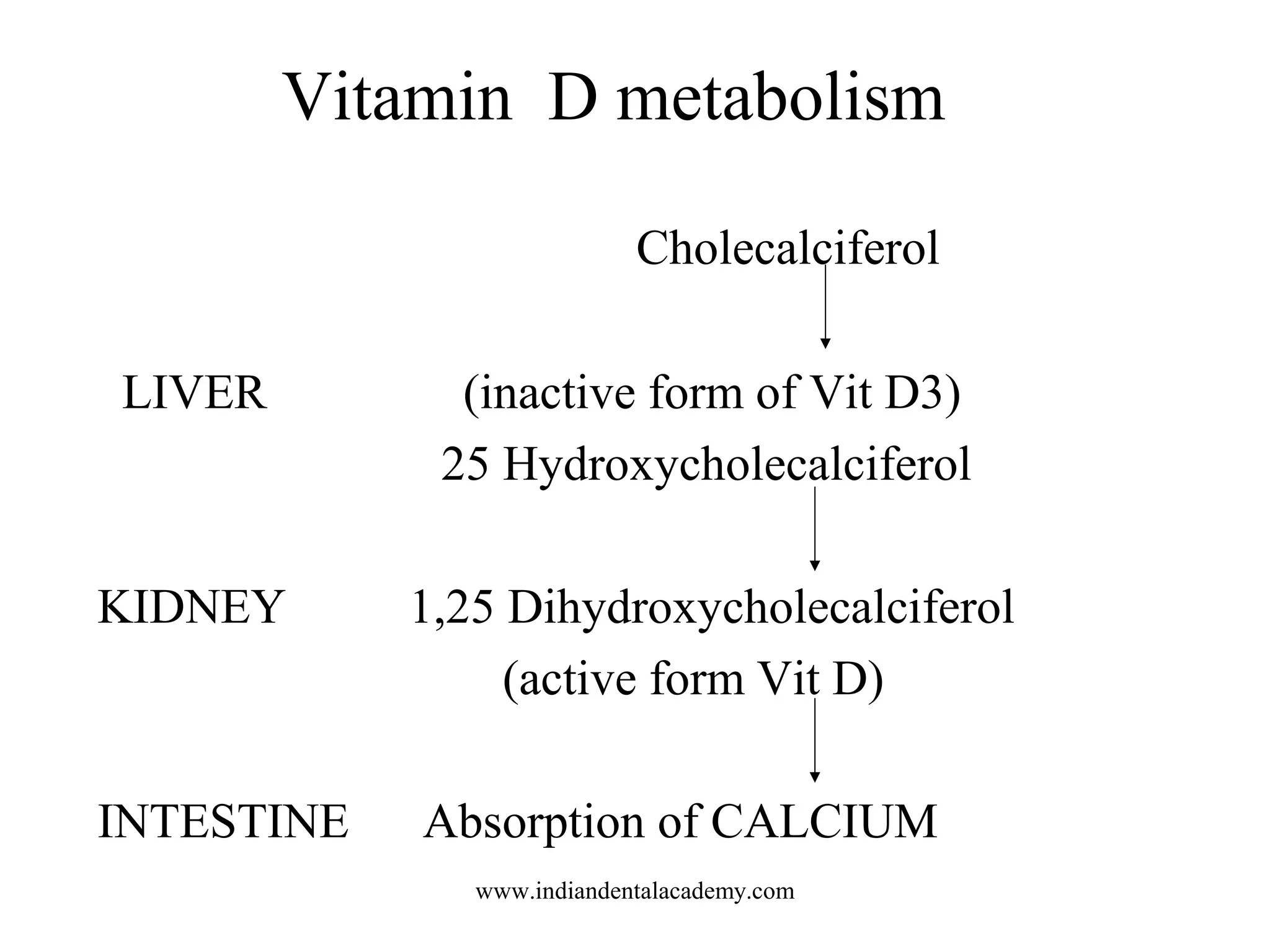
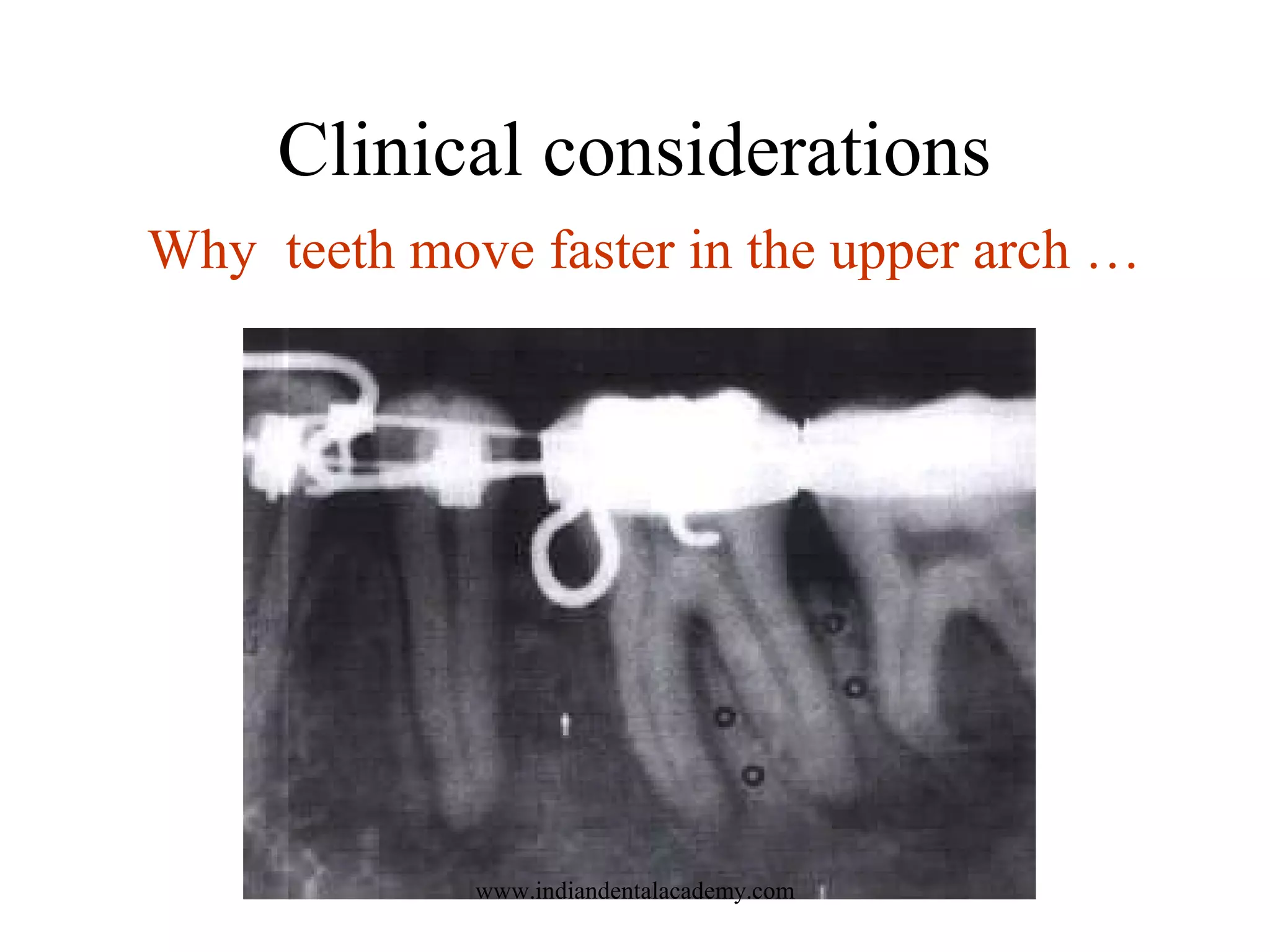
The document details the classification, morphology, histology, development, and remodeling of bones, emphasizing the importance of metabolic factors in orthodontics. It outlines various types of bone formation, such as intramembranous and endochondral ossification, and discusses the influence of mechanical stress on bone architecture. Additionally, it highlights clinical considerations in orthodontics, including factors affecting tooth movement and the implications of conditions like osteoporosis and periodontal disease on dental treatment.