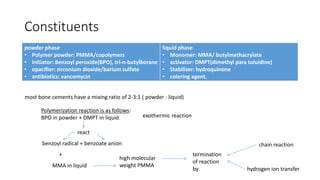
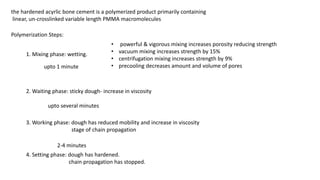
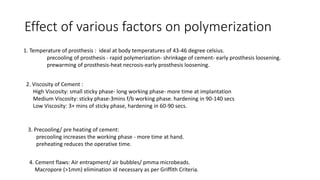
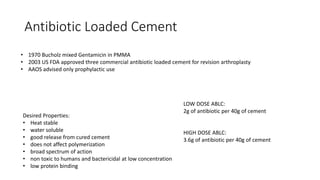
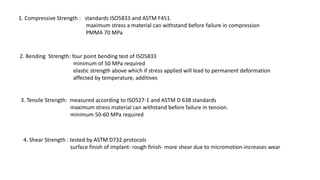
Bone cements have been used since the late 19th century to anchor orthopedic implants. They are composed of PMMA powder mixed with MMA liquid monomer. The exothermic polymerization reaction produces hardened acrylic cement anchoring implants. Key developments included the use of centrifugation and vacuum mixing to reduce porosity. Antibiotic-loaded cement was introduced in the 1970s. Compressive strength above 70MPa is required. Complications include bone cement implantation syndrome occurring during implantation. Removal requires careful techniques to avoid bone loss.