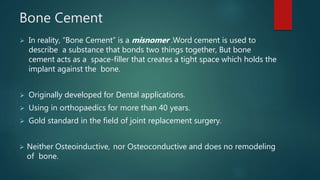
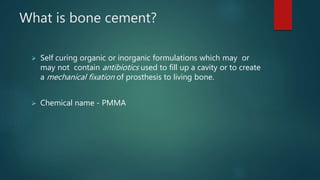
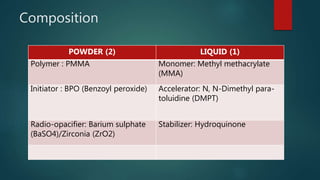
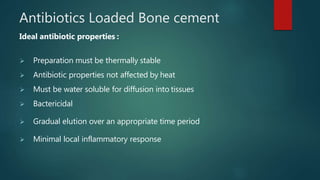
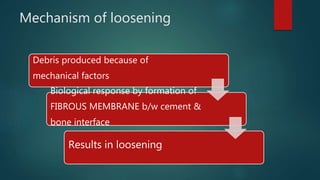
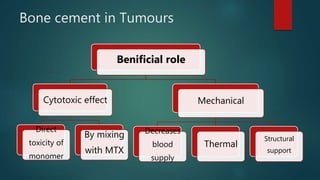
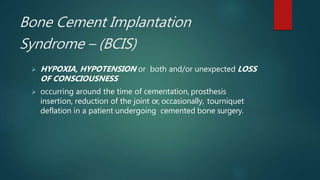
Bone cement is a misnomer as it does not bond bone, but rather fills space to secure prosthetic implants. Originally developed for dentistry, it has been used in orthopedics for over 40 years. It is made of PMMA powder and MMA liquid that polymerize during mixing to form a hardened mass. Precise techniques are used for mixing and delivering the cement to reduce porosity and ensure a secure fit. Cemented joint replacements can loosen over time from debris at cement-bone interfaces. Antibiotics can be added to prevent infection. Potential issues include temperature rise and release of substances that can cause hypotension during surgery.

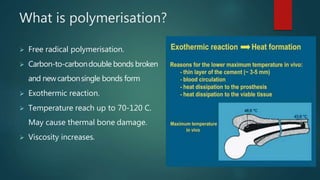

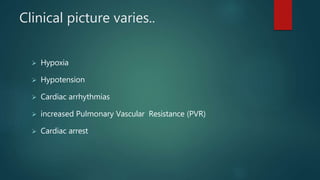
![Classification
• Grade 1: moderate hypoxia (SpO2-94%) or hypotension [fall
in systolic blood pressure (SBP) 20%].
• Grade 2: severe hypoxia (SpO2-88%) or hypotension (fall in
SBP 40%) or unexpected loss of consciousness.
• Grade 3: cardiovascular collapse requiring CPR.](https://image.slidesharecdn.com/bonecement-191027092448/85/Bone-cement-37-320.jpg)