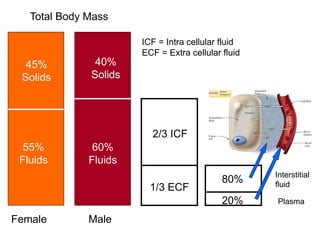
1. The normal composition of body fluids consists of 55% fluids and 45% solids in males, and 60% fluids and 40% solids in females. Total body water is divided into intracellular fluid (ICF) and extracellular fluid (ECF).
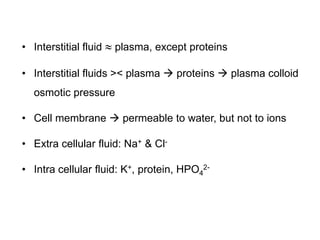
2. ECF contains plasma, interstitial fluid, and transcellular fluids such as lymph and cerebrospinal fluid. ICF volume is about 28L and ECF volume is about 14L in adults.
3. Fluid volumes are regulated through osmosis driven by electrolyte concentrations between compartments. Imbalances can cause conditions such as edema. Hormones and renal control maintain fluid homeostasis.