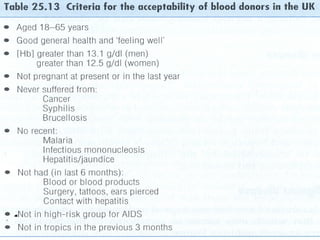
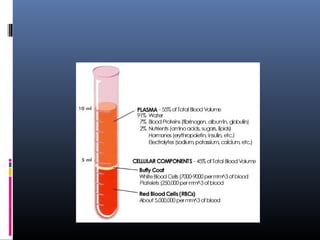
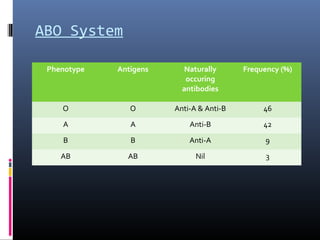
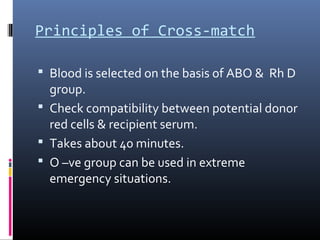
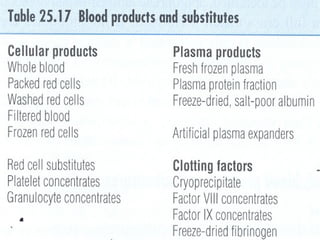
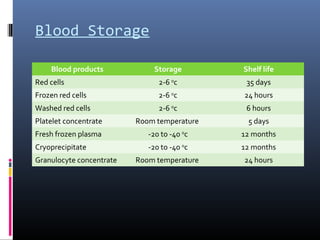
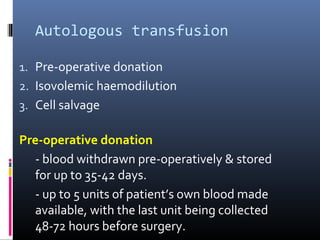
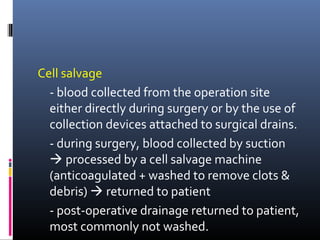
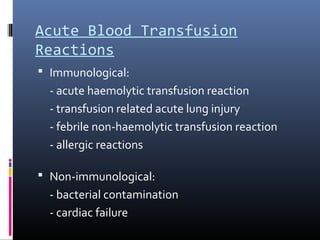
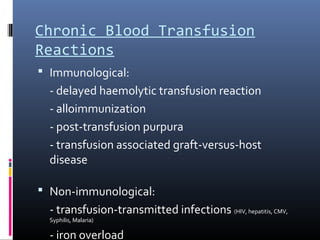
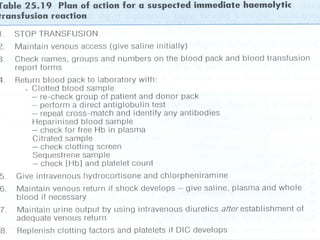
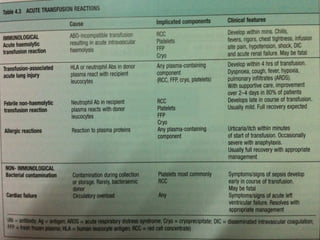
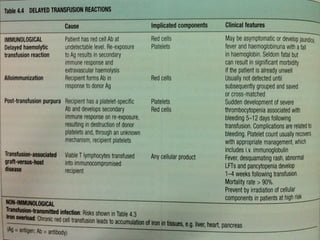
This document summarizes information about blood transfusions, including the different components that can be transfused and their indications. It discusses the major blood group systems, principles of blood typing and cross-matching to ensure compatibility. Safety considerations for donors and recipients are covered, as well as potential acute and chronic transfusion reactions. A variety of blood products are described, such as red blood cell concentrates, platelets, fresh frozen plasma and cryoprecipitate, along with their typical storage times.