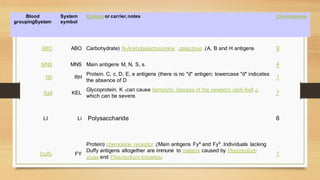
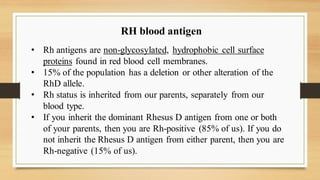
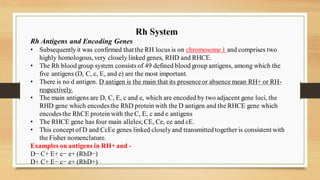
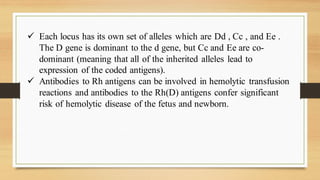
The ABO blood antigens are carbohydrates linked to cell surface proteins that are synthesized by polymorphic glycosyltransferase enzymes. There are three allelic variants of this gene that determine blood type: type O has no enzymatic activity, type A adds N-acetylgalactosamine, and type B adds galactose. Rh antigens are non-glycosylated proteins found in red blood cells and determine Rh factor. Anti-RhD antibodies can cause hemolytic disease of the newborn by destroying fetal red blood cells if the mother is Rh-negative and carries an Rh-positive fetus.