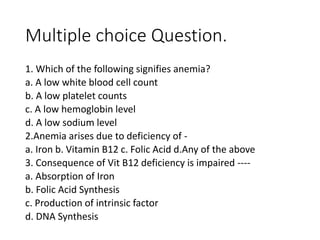
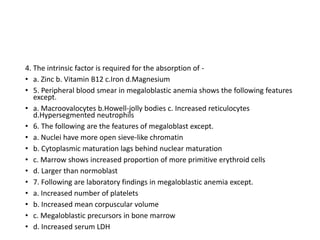
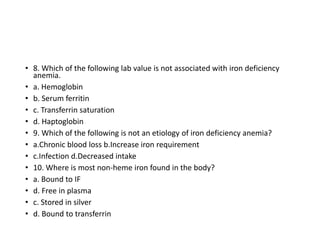
Iron deficiency anemia is a common type of anemia caused by low iron levels. It develops when iron loss from bleeding or inadequate dietary iron intake exceeds the amount the body absorbs. Symptoms include fatigue, pale skin, shortness of breath, and irregular heartbeat. Diagnosis involves blood tests to measure hemoglobin and iron levels. Treatment focuses on oral iron supplements and improving iron intake through diet.