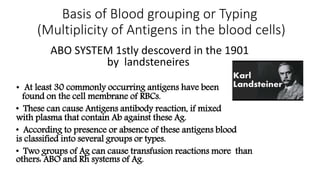
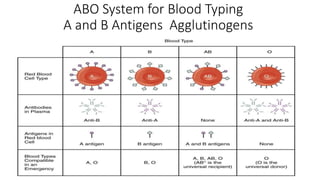
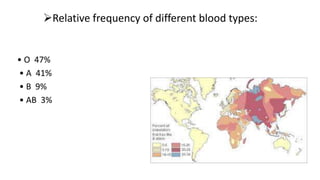
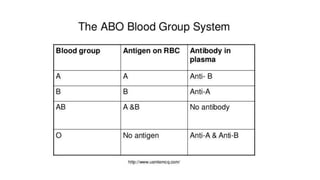
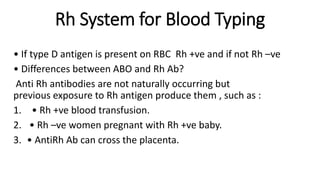
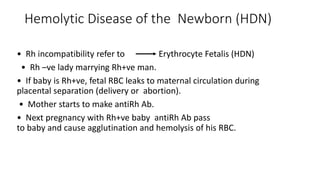
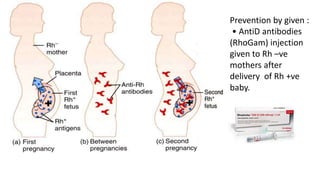
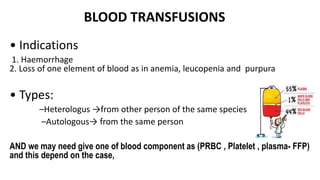
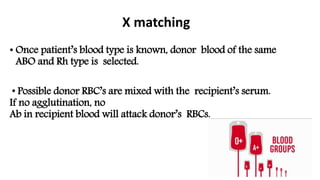
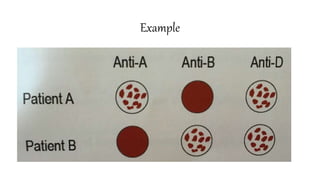
This document discusses blood typing and blood transfusions. It describes the ABO and Rh blood typing systems, which are important for preventing transfusion reactions. The ABO system categorizes blood based on the presence of A and B antigens, while the Rh system distinguishes Rh+ and Rh- blood based on the D antigen. Cross-matching tests ensure a donor's blood is compatible with a recipient's before transfusion to avoid hemolysis or other reactions from antigen-antibody incompatibility. Proper blood typing and cross-matching are essential for safe blood transfusions.