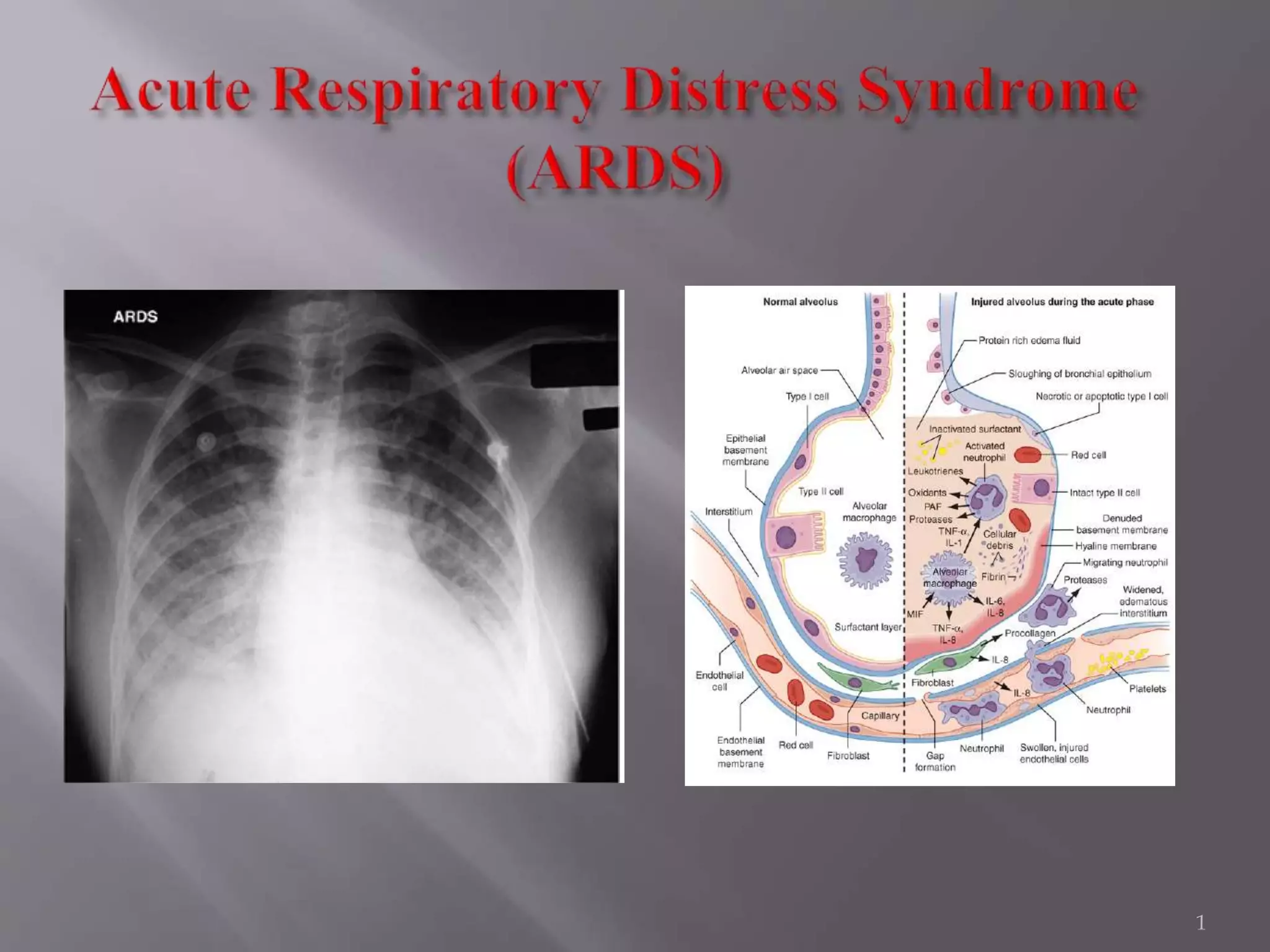
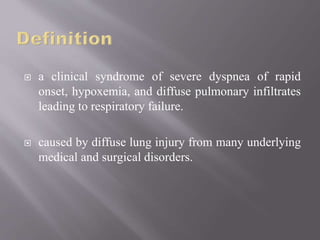
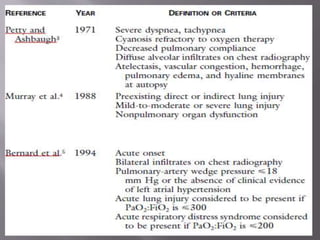
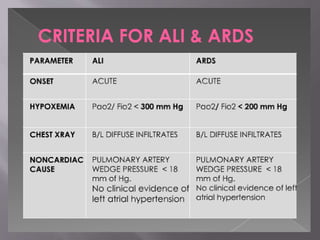
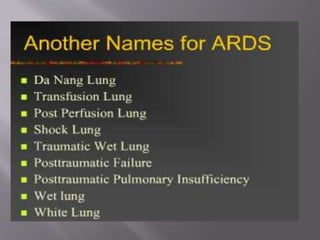
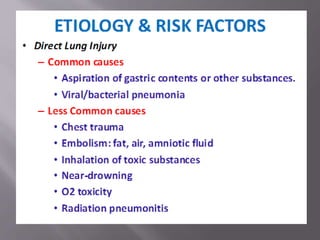
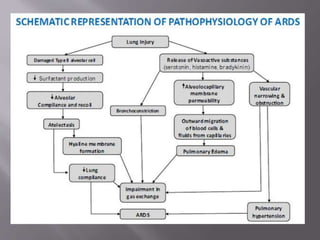
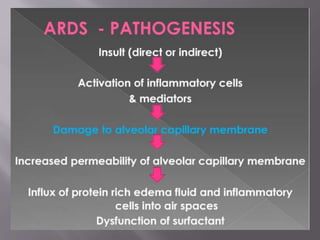
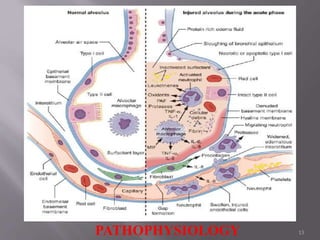
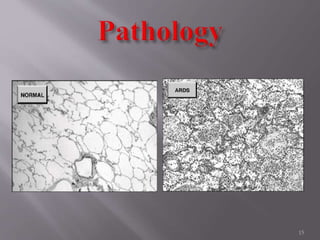
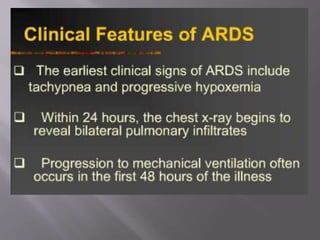
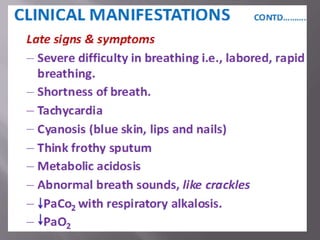
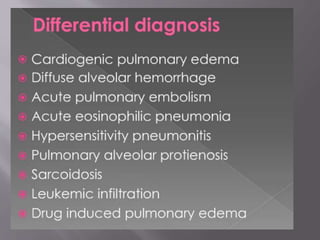
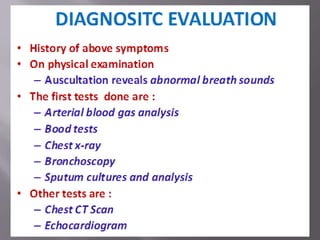
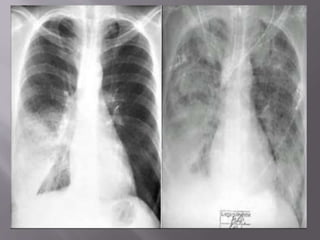
1. Acute respiratory distress syndrome (ARDS) is a clinical syndrome characterized by rapid onset of severe breathing difficulties, low oxygen levels in blood, and diffuse lung inflammation and fluid buildup leading to respiratory failure.
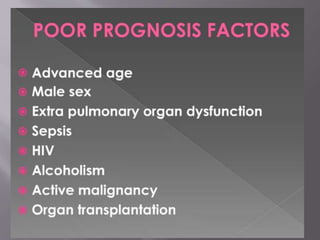
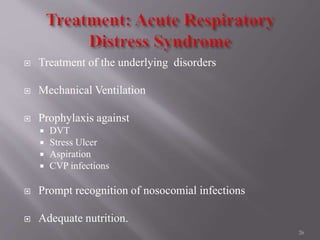
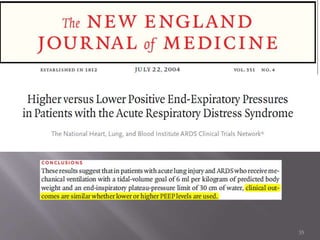
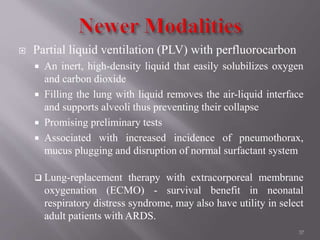
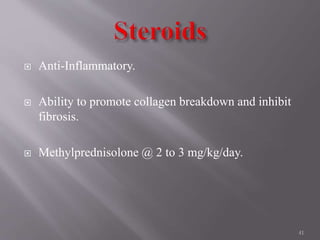
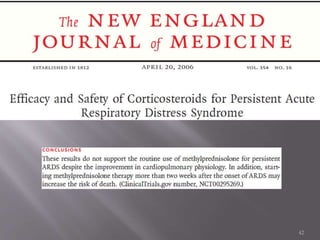
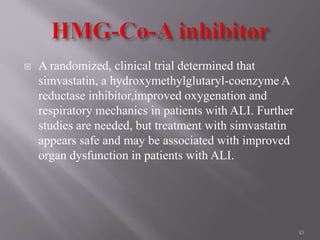
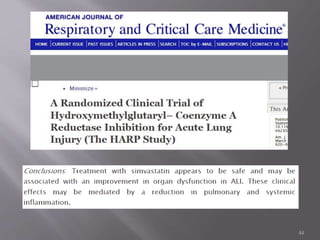
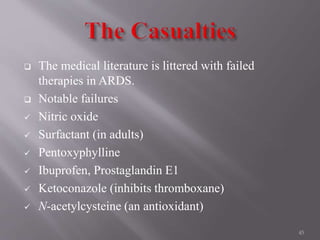
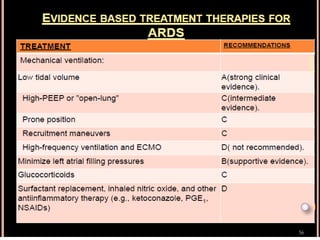
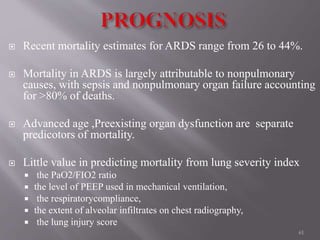
2. ARDS has many underlying causes and results from diffuse lung injury. While research has studied many potential treatments, ARDS remains untreatable and mortality remains high.
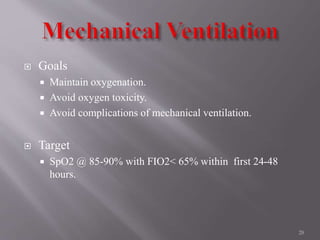
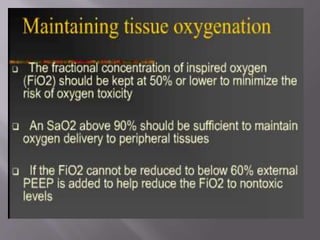
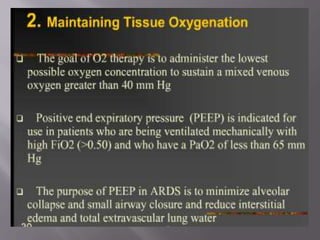
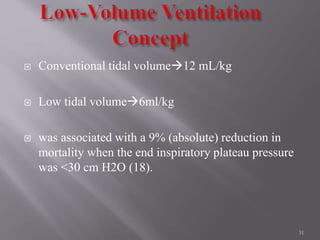
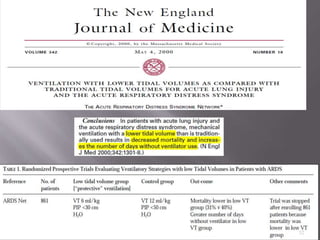
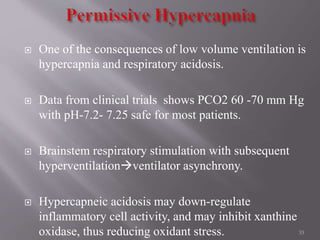
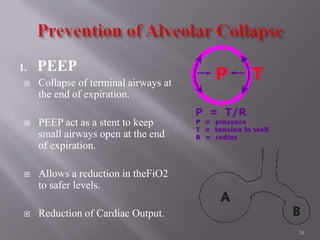
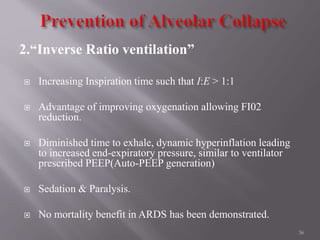
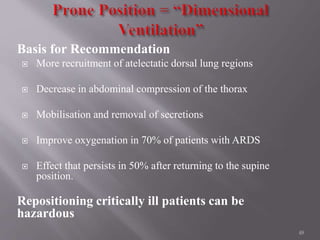
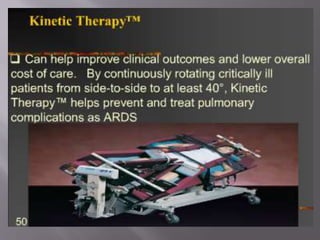
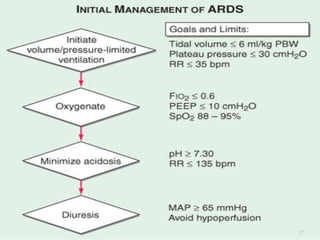
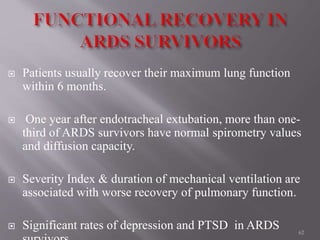
3. Ventilator management to prevent lung injury without compromising oxygen levels is the main supportive treatment for ARDS.