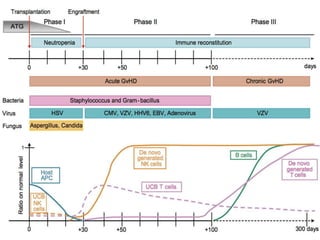
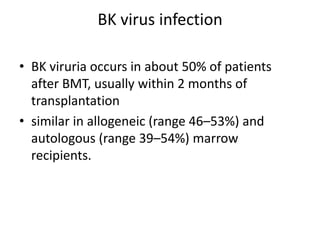
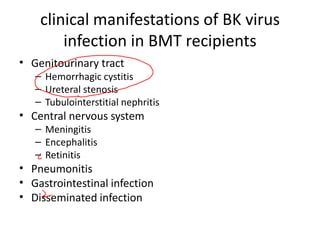
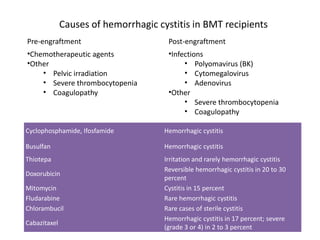
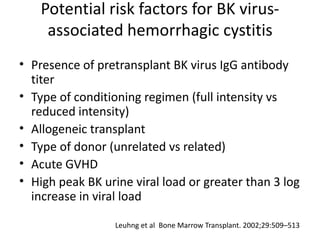
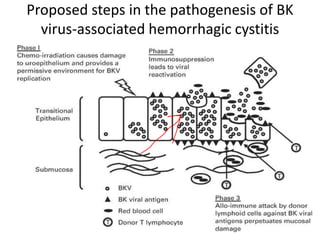
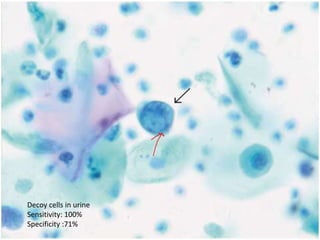
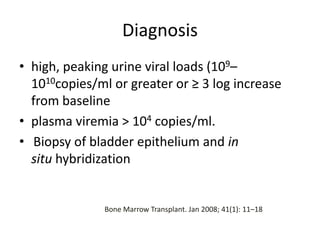
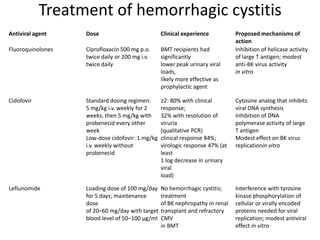
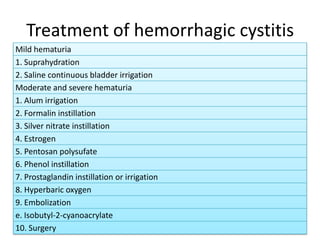
The document discusses BK virus infection in hematopoietic stem cell transplant (HSCT) patients, emphasizing its prevalence, clinical manifestations, and potential complications such as hemorrhagic cystitis. It outlines causes, risk factors, diagnosis, and treatment options for BK-associated conditions, highlighting antiviral therapies and management strategies. Key preventive measures like fluoroquinolone antibiotics and other therapeutic agents like cidofovir and leflunomide are also mentioned.