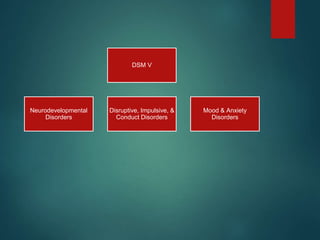
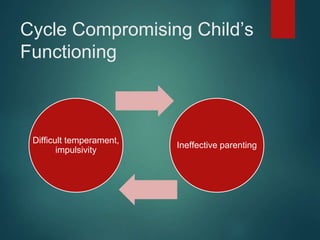
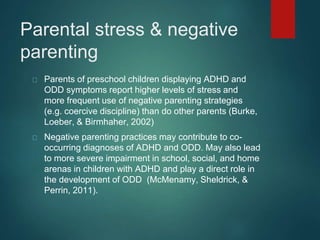
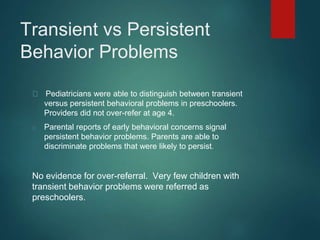
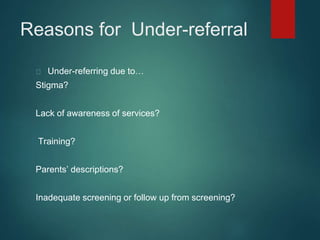
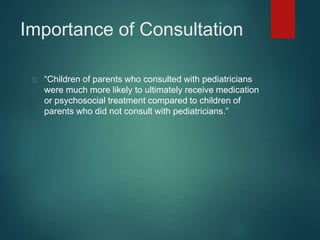
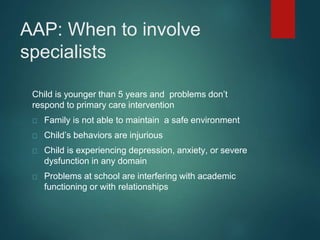
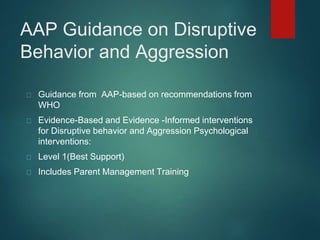
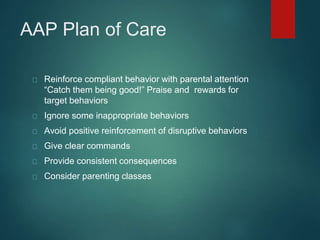
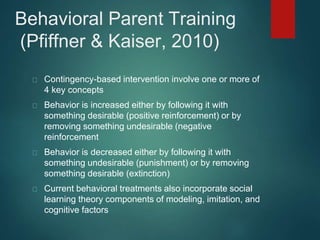
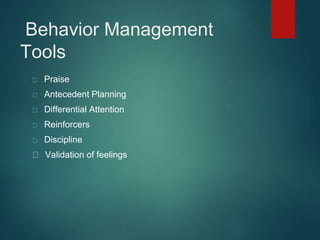
The document discusses behavioral interventions for children with ADHD, ODD, ASD, and other behavior challenges, emphasizing the importance of early intervention and effective parenting strategies. It outlines the critical role of pediatric providers in addressing behavioral concerns and highlights the benefits of parent management training. Evidence-based recommendations and consultation guidelines are provided to improve treatment outcomes and parental engagement in their children's behavioral management.