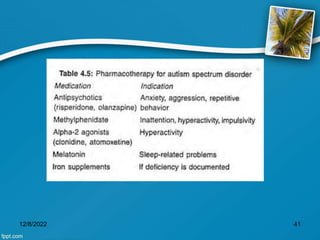
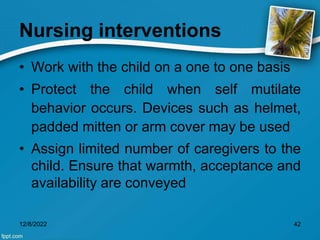
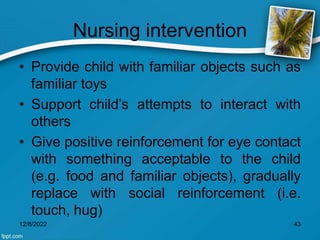
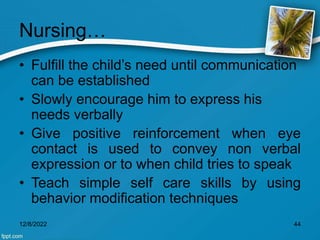
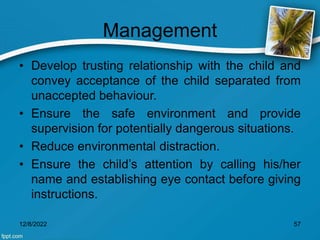
The document provides information on behavioral disorders in children, including oppositional defiant disorder, conduct disorder, and attention deficit hyperactivity disorder. It discusses causes such as genetics, poverty, poor parenting, and media exposure. Symptoms include harming others, property damage, lying, poor school performance, and tantrums. Diagnosis involves history and observation. Treatment includes medication, behavioral therapy, and special schooling. Nursing interventions focus on one-on-one support, positive reinforcement, language training, and ensuring a safe environment.















![Management
• Distraction and 'time out' techniques are useful.
• Providing a safe setting. Many children have
difficulty stopping tantrums on their own.
• A time-out technique, in which the child must sit
alone in a dull place (a corner or room [other than
the child’s bedroom] that is not dark or scary and has
no television or toys) for a brief period, is a good
approach to altering unacceptable behavior.
12/8/2022 118](https://image.slidesharecdn.com/behavioraldisorder-221208152457-e803ae0e/85/Behavioral-Disorder-ppt-118-320.jpg)



![Juvenile Delinquency
• Children who show oppositional defiant behavior
or conduct disorders and come into conflict with the
juvenile justice system are called juvenile delinquents.
• also known as "juvenile offending", is the act of
participating in unlawful behavior as a minor or
individual younger than the statutory age of majority.
• Juvenile crimes can range from status offenses (such
as underage smoking/drinking), to property
crimes and violent crimes.[3]
12/8/2022 145](https://image.slidesharecdn.com/behavioraldisorder-221208152457-e803ae0e/85/Behavioral-Disorder-ppt-145-320.jpg)
![REFERENCES
1. The Most Common Behavior Disorders in Children [Internet]. Healthline.
2020 [cited 11 October 2020]. Available from:
https://www.healthline.com/health/parenting/behavioral-disorders-in-
children
2. Behavioural disorders in children [Internet]. Betterhealth.vic.gov.au.
2020 [cited 11 October 2020]. Available from:
https://www.betterhealth.vic.gov.au/health/healthyliving/behavioural-
disorders-in-children
3. Behavior or Conduct Problems in Children | CDC [Internet]. Centers for
Disease Control and Prevention. 2020 [cited 11 October 2020].
Available from:
https://www.cdc.gov/childrensmentalhealth/behavior.html
4. Everything You Need to Know About ADHD [Internet]. Healthline. 2020
[cited 11 October 2020]. Available from:
https://www.healthline.com/health/adhd#:~:text=Attention%20deficit%20
hyperactivity%20disorder%20(ADHD,and%20children%20can%20have
%20ADHD.
5. Ghai O, Paul V, Bagga A. Essential Pediatrics. 7th ed. CBS
Publisher&Distributers; 2008.
12/8/2022 159](https://image.slidesharecdn.com/behavioraldisorder-221208152457-e803ae0e/85/Behavioral-Disorder-ppt-159-320.jpg)