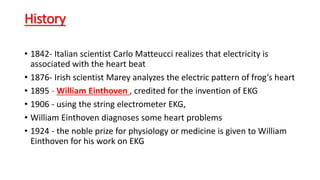
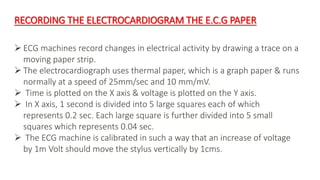
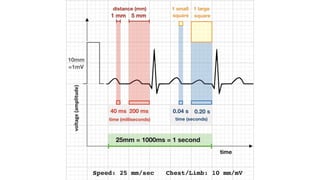
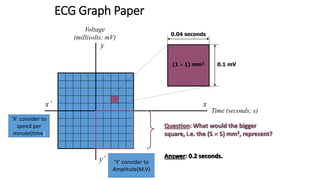
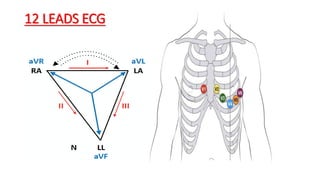
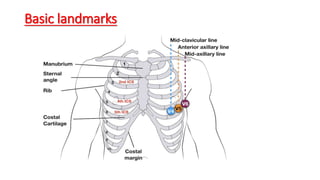
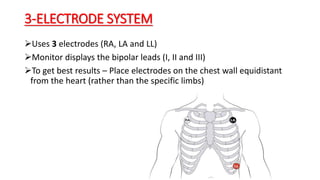
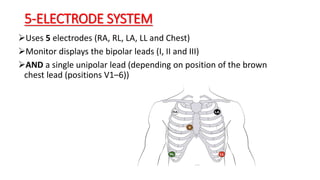
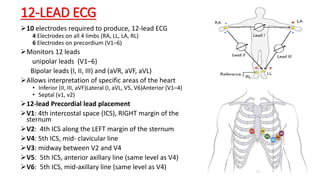
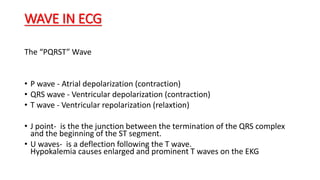
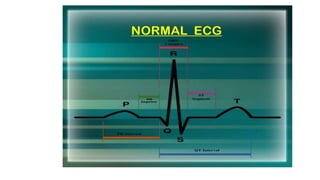
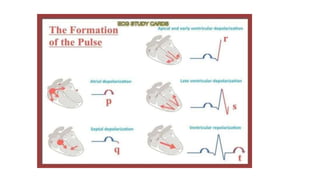
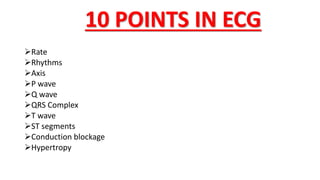
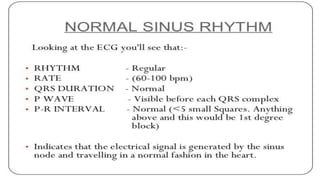
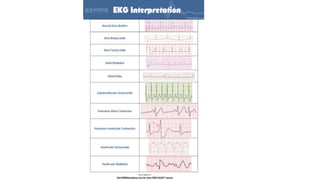
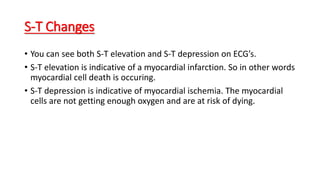
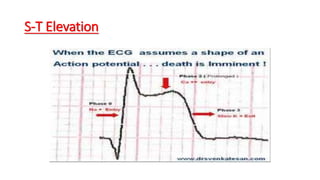
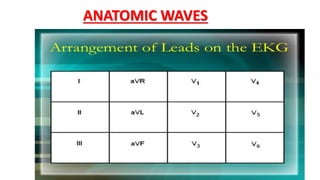
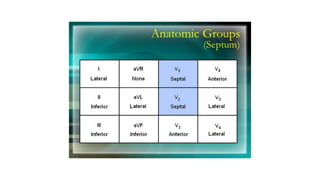
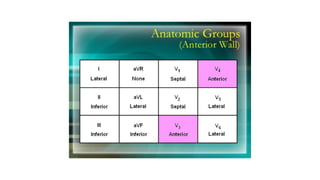
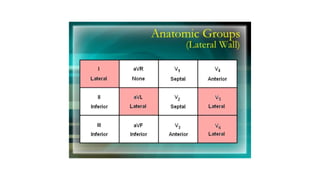
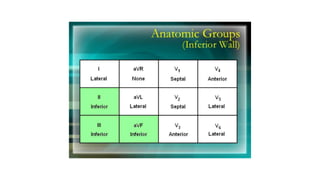
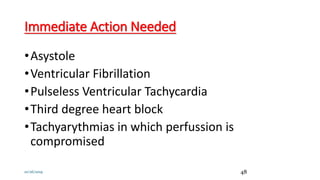
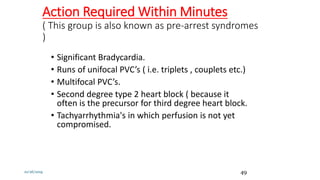
The document provides an outline for a lecture on basic electrocardiograms (ECGs). It discusses the history of ECGs, outlines the standardization of ECGs, and explains the reasons for performing ECGs. It also describes the 12-lead ECG system and proper electrode placement. Key aspects of ECG waves and rhythms are defined. Ten assessment points for ECGs are identified. Finally, the document categorizes cardiac rhythms according to the required intervention hierarchy.