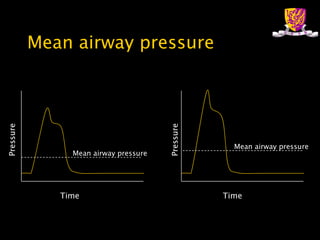
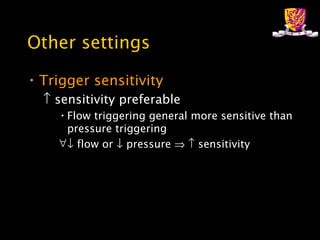
This document provides an overview of basic mechanical ventilation. It discusses how oxygen is delivered and carbon dioxide is removed from the lungs through factors like FiO2, mean alveolar pressure, ventilation, and respiratory rate. It also covers settings like inspiratory time, PEEP, trigger sensitivity, and rise time. Complications of mechanical ventilation like barotrauma, gas trapping, and their causes are summarized. The effects on cardiovascular system are briefly discussed. Specific ventilation modes require downloading separate lectures.