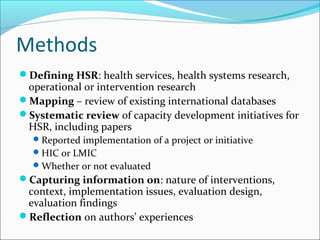
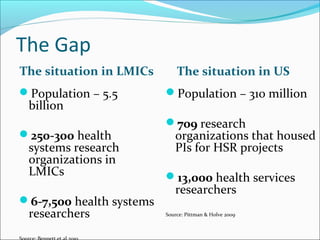
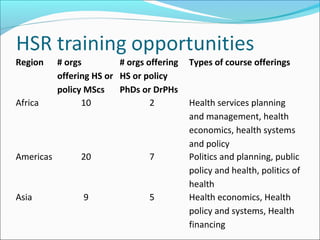
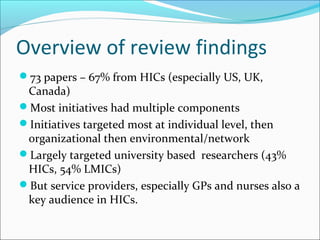
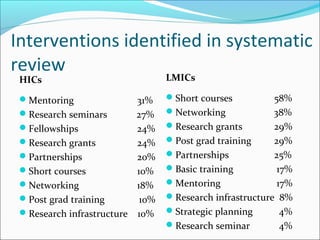
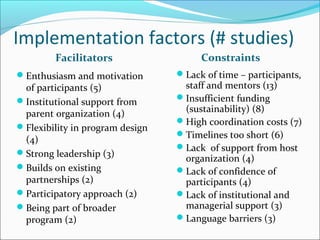
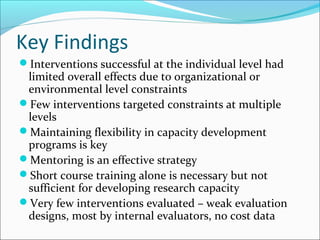
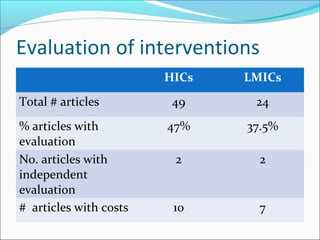
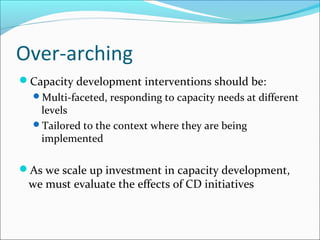
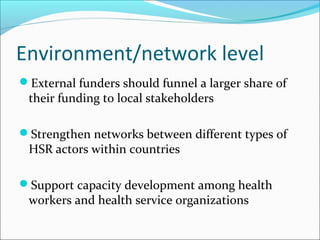
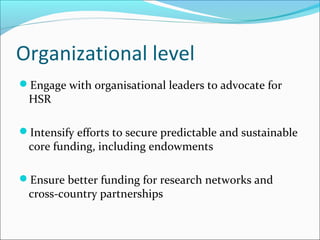
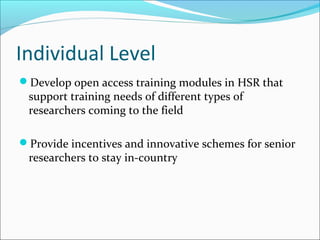
The document aims to map health services research (HSR) capacity across individual, organizational, and environmental levels and identify effective strategies for capacity development. It reviews existing databases and initiatives related to HSR, highlighting various interventions and their success factors and constraints, particularly in low- and middle-income countries (LMICs) versus high-income countries (HICs). Key findings indicate that while individual-level interventions are prevalent, they often have limited overall effectiveness due to higher-level constraints, underscoring the need for multi-faceted and context-tailored approaches in capacity development.