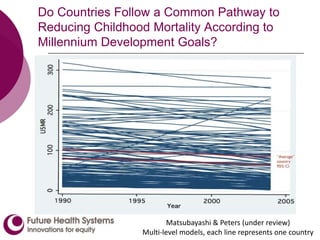
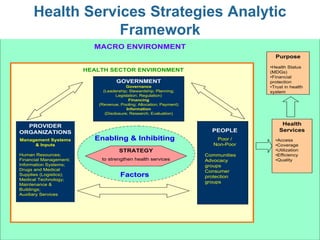
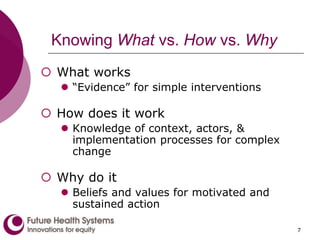
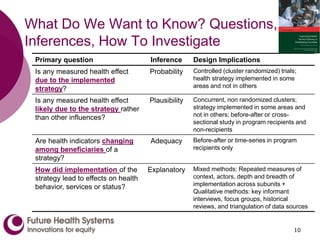
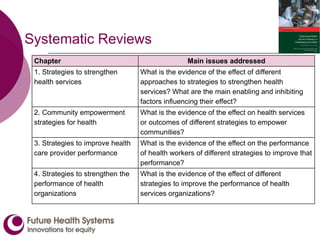
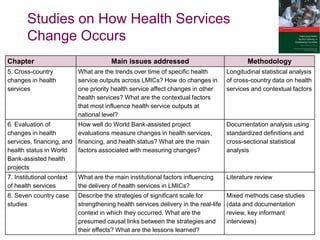
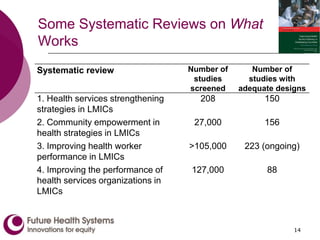
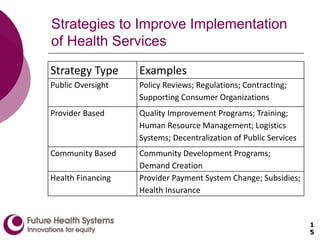
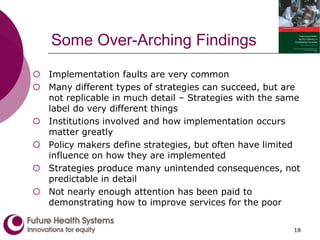
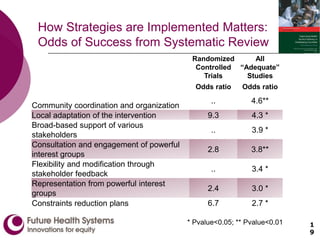
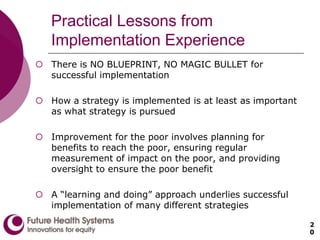
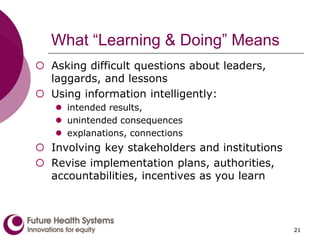
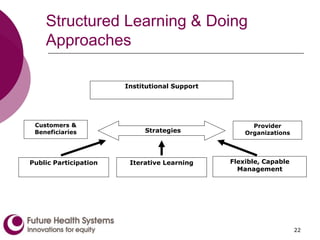
The document discusses strategies and evidence for improving health service delivery in developing countries, focusing on methods that enhance effectiveness and implementation. Key topics include understanding health service strategies, community empowerment, and the performance of health workers and organizations. The findings emphasize the importance of context, stakeholder involvement, and continuous learning in implementing successful health interventions, particularly for the poor and disadvantaged.